CALL TODAY 646-933-3224 | EMAIL

Surgical Precision, Compassionate Care


Surgical Experts Dedicated to Improving Lives
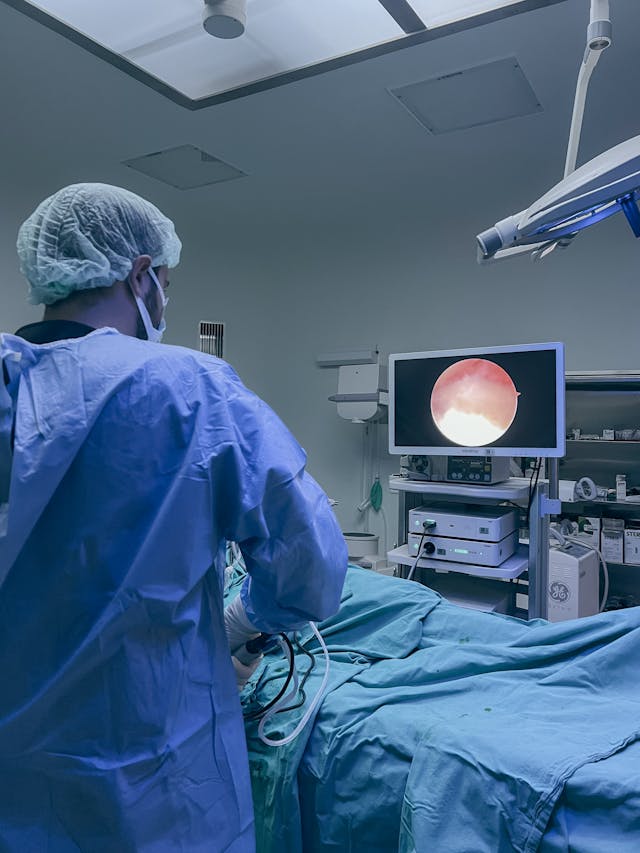
At Lenox Hill Surgeons LLP, our dedicated surgeons and medical professionals provide compassionate care with the highest ethical & professional standards. In our state of the art facility, we offer surgical services using only the most cutting edge and current procedures and treatments. We specialize in general surgery, with special expertise in minimally invasive surgery. Minimally invasive surgery typically allows patients to experience easier recovery than traditional open surgery. It also allows for more precise and less traumatic surgery. When minimally invasive surgery is not an option, we are also highly experienced in traditional open surgical procedures.
Our doctors are experienced and skilled surgeons having undergone extensive training in school, residency and fellowships. They all practice medicine with ethically, compassionately and have superb bedside manner. In the operating room they all exhibit precision mechanical abilities, analytical thinking and the ability to visualize tissue in three dimensions. These skills allow our surgeons to be some of the most dexterous and skilled professionals in New York City.
Call us: 646-933-3224
Conditions We Treat
What You Can Expect From Us
1. Direct Access to Your Surgeon
- Same-day or next-day consultations (in-person or virtual)
- 24-hour access to your surgeon with rapid response times
- One surgeon throughout your entire care process
2. Streamlined Scheduling and Navigation
- Expedited pre-operative testing and OR booking
- Full coordination with primary care and specialty providers
- Dedicated concierge coordinator to handle logistics and paperwork
3. Pre- and Post-Operative White-Glove Services
- Optional pre-operative in-home or telehealth consultations
- Post-operative home check-ins by nurse or physician assistant
- Access to private recovery suites or luxury post-op facilities
4. Robotic and Minimally Invasive Surgical Expertise
- State-of-the-art procedures including hernia repair, gallbladder removal, abdominal wall reconstruction, GERD treatment, and colon surgery
Visit our main website at https://LenoxHillSurgeons.com/
Blog Posts are Below:
Understanding Breast Surgery Options
Understanding breast surgery options is an important step for patients who are considering surgical treatment for medical, cosmetic, or reconstructive reasons. Breast surgery can address a wide range of concerns, from cancer treatment and risk reduction to symptom relief and aesthetic goals. Knowing the different procedures available, why they are performed, and what to expect can help patients make informed and confident decisions about their care.

Reasons Patients Consider Breast Surgery
Breast surgery is not a one-size-fits-all solution. Patients pursue surgical treatment for many different reasons, including health-related needs and quality-of-life improvements. Common reasons include:
- Treatment or prevention of breast cancer
- Evaluation or removal of suspicious breast masses
- Chronic pain caused by large or heavy breasts
- Reconstruction following mastectomy or lumpectomy
- Correction of congenital or developmental breast conditions
Each patient’s goals, diagnosis, and overall health play a role in determining the most appropriate surgical approach.
Breast Surgery for Cancer Treatment
Breast cancer surgery is one of the most common reasons patients seek surgical care. The type of surgery recommended depends on factors such as tumor size, location, stage of cancer, and patient preference.
- Lumpectomy: Also known as breast-conserving surgery, this procedure removes the tumor and a small margin of surrounding tissue while preserving most of the breast.
- Mastectomy: Involves removal of the entire breast and may be recommended for larger tumors, multiple tumors, or patients at high risk of recurrence.
- Sentinel Lymph Node Biopsy: Used to determine whether cancer has spread to nearby lymph nodes.
- Axillary Lymph Node Dissection: Removal of multiple lymph nodes when cancer spread is suspected or confirmed.
Advancements in surgical techniques have allowed for more targeted procedures that prioritize both cancer control and cosmetic outcomes.
Preventive and Risk-Reducing Breast Surgery
Some patients with a strong family history of breast cancer or known genetic mutations choose preventive breast surgery to significantly reduce their risk. Prophylactic mastectomy may be recommended in select cases after thorough evaluation and counseling. This approach can dramatically lower the risk of developing breast cancer and is often combined with immediate or delayed breast reconstruction.
Breast Reconstruction Options
Breast reconstruction surgery helps restore the shape and appearance of the breast following mastectomy or lumpectomy. Reconstruction can be performed at the time of cancer surgery or at a later date, depending on the patient’s treatment plan and personal preference.
Common reconstruction options include:
- Implant-Based Reconstruction: Uses saline or silicone implants to recreate breast shape.
- Autologous (Flap) Reconstruction: Uses the patient’s own tissue, often taken from the abdomen or back, to reconstruct the breast.
- Combination Reconstruction: Incorporates both implants and natural tissue for optimal contour and support.
Each method has unique benefits and considerations related to recovery time, appearance, and long-term results.
Breast Surgery for Benign Conditions
Not all breast surgeries are related to cancer. Many patients require surgical treatment for non-cancerous conditions that cause discomfort or concern. These include:
- Removal of benign breast lumps or cysts
- Excision of abnormal biopsy findings
- Treatment of breast infections or abscesses
- Correction of breast asymmetry or deformities
In these cases, surgery is often minimally invasive and focuses on symptom relief and peace of mind.
What to Expect Before and After Breast Surgery
Before surgery, patients typically undergo imaging studies, lab testing, and a detailed consultation to review risks, benefits, and expected outcomes. Recovery time varies based on the procedure performed but may include:
- Temporary soreness or swelling
- Activity restrictions during healing
- Drain placement in some procedures
- Follow-up visits to monitor recovery
Most patients are able to return to normal daily activities within a few weeks, especially with modern surgical techniques and proper post-operative care.
Making the Right Choice for Your Breast Health
Choosing the right breast surgery option requires personalized evaluation and open communication with your surgical team. Every patient’s anatomy, diagnosis, and goals are unique, and treatment plans should reflect those individual needs. With early diagnosis, advanced techniques, and comprehensive care, breast surgery can offer both effective treatment and long-term reassurance.
If you are exploring breast surgery options or have concerns about breast health, professional evaluation is the first step. Our surgical team provides thorough consultations, advanced diagnostic services, and a full range of breast surgery solutions tailored to your needs. Contact us today to schedule a consultation or to learn more about your available options.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Prostate Health and Surgery Options
Prostate health and surgery options are important topics for men, especially as prostate conditions become more common with age. The prostate is a small gland that plays a key role in male reproductive health, but it can also be the source of a range of medical issues that affect urinary function, sexual health, and overall quality of life. Understanding common prostate conditions and the available surgical treatments can help men make informed decisions about their care.
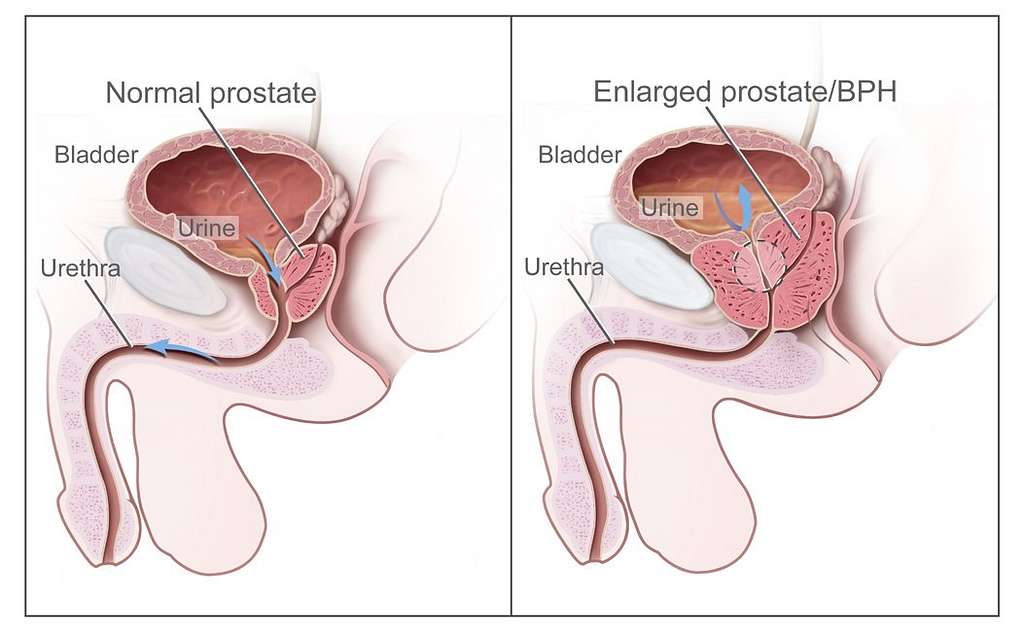
Understanding the Role of the Prostate
The prostate gland sits just below the bladder and surrounds the urethra, the tube that carries urine out of the body. Its primary function is to produce seminal fluid that nourishes and transports sperm. Because of its location, even small changes in prostate size or structure can significantly affect urinary flow and bladder control.
As men age, the prostate naturally changes, increasing the likelihood of benign or malignant conditions that may require medical or surgical intervention.
Common Prostate Conditions
Several conditions can impact prostate health, each with different symptoms and treatment approaches:
- Benign Prostatic Hyperplasia (BPH): A non-cancerous enlargement of the prostate that commonly causes urinary frequency, weak urine stream, difficulty starting urination, and nighttime urination.
- Prostatitis: Inflammation or infection of the prostate, often causing pelvic pain, painful urination, or flu-like symptoms.
- Prostate Cancer: One of the most common cancers in men, often detected through prostate-specific antigen (PSA) testing and biopsy.
While some prostate conditions can be managed with medication or lifestyle changes, others may require surgical treatment to relieve symptoms or remove diseased tissue.
When Surgery Becomes Necessary
Surgery is typically recommended when conservative treatments are no longer effective or when the condition poses a risk to long-term health. For example, severe urinary obstruction from BPH can lead to bladder damage or kidney problems if left untreated. In the case of prostate cancer, surgery may be necessary to remove the cancer and prevent its spread.
Symptoms that may indicate the need for surgical evaluation include:
- Persistent difficulty urinating
- Inability to fully empty the bladder
- Recurrent urinary tract infections
- Blood in the urine
- Elevated PSA levels or abnormal biopsy results
Prostate Surgery Options
Advances in medical technology have significantly improved prostate surgery options, making procedures safer and less invasive than in the past. Common surgical approaches include:
- Transurethral Resection of the Prostate (TURP): A well-established procedure for treating BPH by removing excess prostate tissue through the urethra.
- Laser Prostate Surgery: Uses laser energy to remove or shrink prostate tissue, often resulting in less bleeding and faster recovery.
- Simple Prostatectomy: Recommended for very large prostates causing severe symptoms; removes the inner portion of the prostate.
- Radical Prostatectomy: Involves complete removal of the prostate gland and is commonly used to treat localized prostate cancer.
- Robotic-Assisted Prostate Surgery: A minimally invasive approach that offers enhanced precision, smaller incisions, reduced pain, and shorter recovery times.
The choice of procedure depends on the patient’s diagnosis, prostate size, overall health, and personal treatment goals.
What to Expect After Prostate Surgery
Recovery after prostate surgery varies depending on the procedure performed. Many minimally invasive surgeries allow patients to return home within a short period and resume light activities within days. Temporary side effects may include urinary leakage, erectile dysfunction, or discomfort, which often improve with time and proper follow-up care.
Post-surgical care typically includes:
- Short-term use of a urinary catheter
- Activity restrictions during healing
- Follow-up visits to monitor recovery
- Pelvic floor exercises to improve urinary control
Most patients experience significant improvement in urinary symptoms and overall quality of life following successful treatment.
Protecting and Monitoring Prostate Health
Proactive prostate care is essential, even before symptoms develop. Regular checkups, PSA testing when appropriate, and discussing urinary or sexual health concerns early can lead to earlier diagnosis and more treatment options. Maintaining a healthy lifestyle — including regular exercise, balanced nutrition, and weight management — also supports long-term prostate health.
Take the Next Step Toward Better Prostate Health
If you’re experiencing urinary symptoms, have concerns about prostate enlargement, or need guidance on prostate cancer treatment options, professional evaluation is key. Our surgical team offers comprehensive prostate care using advanced diagnostic tools and modern surgical techniques tailored to each patient’s needs.
Reach out today to schedule a consultation and learn more about the most effective prostate health and surgery options available.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
How to Know If You Really Have a Hernia
Knowing how to tell if you really have a hernia is essential for seeking the right treatment and preventing complications. Many people experience abdominal or groin discomfort without realizing these symptoms may point to an underlying hernia. Because hernias can worsen over time, early recognition allows for timely evaluation and intervention, which can improve long-term outcomes.

What Exactly Is a Hernia?
A hernia occurs when an internal organ or tissue pushes through a weak spot in the surrounding muscle or connective tissue. This weakness may be present from birth or may develop gradually due to strain, injury, or surgery. Hernias can occur in several areas of the body, but the most common include:
- Inguinal Hernias: Located in the groin, more common in men.
- Femoral Hernias: Occur lower in the groin, more common in women.
- Umbilical Hernias: Develop near the belly button.
- Incisional Hernias: Appear near previous surgical incisions.
- Hiatal Hernias: Involve part of the stomach pushing into the chest cavity.
Understanding the type of hernia you may have helps guide what symptoms to watch for.
Common Symptoms of a Hernia
While symptoms vary depending on location and severity, certain signs strongly suggest the presence of a hernia. Key symptoms include:
- A Noticeable Bulge: One of the most recognizable signs. The bulge may become more prominent when standing, coughing, or lifting heavy objects.
- Discomfort or Pain: Pain may range from mild pressure to sharp, persistent pain. Activities that increase abdominal pressure often worsen symptoms.
- Heaviness or Weakness in the Abdomen or Groin: Many people describe a dragging or pulling sensation.
- Pain After Eating: Common in hiatal hernias, where stomach tissue pushes upward into the chest cavity.
- Nausea or Digestive Issues: In more advanced cases, the hernia may disrupt normal digestion or bowel movements.
These symptoms often come and go, leading many individuals to ignore them or assume they’re caused by strain, bloating, or muscle injury.
Symptoms That Require Urgent Attention
Some hernias can become trapped (incarcerated) or lose their blood supply (strangulated), posing a medical emergency. Seek immediate care if you experience:
- Severe, worsening abdominal or groin pain
- Nausea and vomiting that does not improve
- A hernia bulge that becomes firm, discolored, or unable to be pushed back in
- Fever or rapid heart rate
These symptoms may signal a blocked or strangulated hernia, requiring emergency surgery.
How Hernias Are Diagnosed
A physical exam is often enough to diagnose most hernias, especially those in the groin or abdominal wall. During the exam, your provider may ask you to stand, cough, or strain to make the hernia more visible.
If further evaluation is needed, diagnostic tools may include:
- Ultrasound: Useful for identifying soft tissue hernias, especially in the groin.
- CT Scan: Provides detailed images of the abdominal wall and internal organs.
- MRI: Helpful in cases where the hernia is small or difficult to detect.
These imaging methods allow for precise diagnosis and help determine the most effective treatment plan.
Is It a Hernia or Something Else?
Various conditions can mimic hernia symptoms, so proper diagnosis is essential. These may include:
- Muscle strains
- Lymph node swelling
- Digestive issues such as acid reflux or bloating
- Testicular conditions in men
- Endometriosis or ovarian issues in women
Because these issues can overlap in symptoms, medical evaluation is the most reliable way to know if you truly have a hernia.
When to Seek Professional Help
If you notice a bulge, persistent discomfort, or recurring abdominal or groin pain, scheduling a medical evaluation is the best next step. Hernias do not heal on their own and can worsen over time. Early diagnosis allows for minimally invasive treatment options and prevents the risk of complications.
Get Clarity and Expert Guidance
If you’re unsure whether your symptoms point to a hernia, a professional assessment can provide answers and peace of mind. Our surgical team offers comprehensive evaluations and personalized treatment plans to help you feel confident and informed about your health.
Contact us today to schedule an appointment and learn more about your options.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Everyday Habits That Increase Your Risk of Hernias
Hernias are a common but often overlooked medical condition that can develop gradually over time due to daily habits that place strain on the abdominal wall. While hernias can occur in anyone, understanding the lifestyle factors and routines that contribute to their formation is key to prevention. By recognizing these risk factors early, you can take steps to protect your health and reduce the likelihood of needing surgical intervention.

What Is a Hernia?
A hernia occurs when an internal organ or tissue pushes through a weak spot in the surrounding muscle or connective tissue. The most common types include inguinal (groin), umbilical (belly button), hiatal (upper stomach), and incisional hernias (near previous surgical sites). Though small hernias may cause mild discomfort, larger ones can lead to serious complications if left untreated.
Everyday Habits That Can Lead to Hernias
Many people don’t realize that routine activities can gradually increase pressure on the abdominal wall, creating or worsening a hernia. Here are some common habits that raise your risk:
- Heavy Lifting Without Proper Technique: One of the leading causes of hernias is lifting heavy objects incorrectly. Bending at the waist instead of using your legs places excessive pressure on your abdominal muscles, increasing the risk of a tear. Always lift with your knees bent and your core engaged.
- Chronic Coughing or Sneezing: Persistent coughing or sneezing from allergies, smoking, or respiratory illnesses can strain the abdominal wall. Over time, this repeated pressure weakens muscles, creating conditions ideal for a hernia to form.
- Poor Posture: Sitting or standing with poor posture for long periods can weaken core muscles. A strong core supports your abdomen and prevents internal tissues from pushing through weak spots.
- Straining During Bowel Movements: Constipation and excessive straining increase intra-abdominal pressure, which can contribute to hernia development, particularly in the groin or lower abdomen. Maintaining a fiber-rich diet and proper hydration helps reduce this risk.
- Obesity and Weight Fluctuations: Carrying extra abdominal weight constantly stresses the muscles and connective tissues of the abdomen. Rapid weight gain or loss can also reduce muscle tone, creating weaknesses where hernias may develop.
- Smoking: Smoking not only contributes to chronic coughing but also interferes with tissue healing and collagen production. This slows muscle repair and weakens the abdominal wall, making hernias more likely to form and harder to heal after surgery.
- Overexertion and Intense Exercise: High-impact workouts, especially those involving heavy weightlifting or sudden twisting motions, can overstretch the abdominal wall if done without proper form or gradual progression.
Who Is Most at Risk?
Certain groups of people are more prone to developing hernias due to physical, occupational, or genetic factors. These include:
- Individuals with a family history of hernias
- People who have had previous abdominal surgery
- Workers who regularly lift or move heavy objects
- Men over the age of 40
- Women who have had multiple pregnancies
Being aware of these risk factors and modifying daily habits can make a significant difference in prevention.
Preventing Hernias Through Healthy Habits
Preventing hernias begins with strengthening your core and reducing abdominal strain. Incorporate these simple but effective habits into your daily routine:
- Engage in regular, low-impact exercise like walking, swimming, or yoga to improve muscle tone.
- Maintain a healthy weight through balanced nutrition and portion control.
- Use proper lifting techniques at work or in the gym.
- Eat plenty of fruits, vegetables, and whole grains to prevent constipation.
- Quit smoking to improve respiratory and tissue health.
Even small changes can help protect your abdominal muscles and reduce the likelihood of a hernia forming or worsening.
Recognizing When to Seek Help
If you experience symptoms such as a visible bulge, pain or discomfort when lifting or bending, nausea, or pressure in the abdomen or groin, it’s important to seek medical evaluation. Early detection allows for less invasive treatment and helps prevent serious complications such as hernia strangulation, which requires emergency surgery.
Protect Your Health with Expert Surgical Care
If you suspect you may have a hernia or are experiencing ongoing abdominal discomfort, a comprehensive evaluation can help determine the best course of treatment. Early diagnosis and, when needed, minimally invasive surgical repair can prevent future complications and restore your comfort and mobility.
Contact our surgical team today to schedule a consultation and discuss effective solutions for hernia prevention and treatment.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
The Future of Surgery: Artificial Intelligence in Surgery
Artificial intelligence (AI) in surgery is revolutionizing the way operations are planned, performed, and monitored. As healthcare continues to integrate advanced technology, the operating room has become one of the most promising environments for AI-driven innovation. From preoperative planning to real-time assistance and post-surgical analysis, AI is reshaping surgical precision and patient outcomes in ways that were once thought impossible.

How Artificial Intelligence is Changing Surgery
Artificial intelligence uses algorithms and machine learning to analyze massive amounts of data and assist surgeons in decision-making. In surgery, this technology can interpret diagnostic images, guide robotic systems, and even predict potential complications before they occur. AI doesn’t replace the surgeon — instead, it enhances their skills and enables more accurate, consistent, and safer results.
Some of the most significant applications of AI in surgery include:
- Preoperative Planning: AI-powered software can analyze medical imaging to identify anatomical structures and abnormalities, helping surgeons plan their approach with precision.
- Intraoperative Assistance: During surgery, AI can assist with navigation, alert the surgeon to risks, and provide real-time feedback through robotic systems.
- Postoperative Monitoring: AI algorithms track patient recovery, monitor for signs of infection, and predict complications before they become critical.
AI and Robotic-Assisted Surgery
Robotic-assisted surgery has already transformed many surgical specialties, offering greater control and flexibility through minimally invasive techniques. The integration of AI takes this advancement even further.
AI-driven surgical robots can “learn” from thousands of previous procedures, using that knowledge to assist with precision tasks such as cutting, suturing, and tissue manipulation. This level of consistency reduces human error, shortens procedure times, and leads to faster patient recovery.
For instance, AI-enhanced systems can identify the boundaries of tissues and blood vessels more accurately than the human eye, minimizing the risk of unintended injury. Surgeons remain fully in control, but AI provides an additional layer of safety and precision.
Benefits of AI in the Operating Room
The benefits of artificial intelligence in surgery extend to both patients and surgical teams. Among the key advantages are:
- Enhanced Accuracy: AI helps identify the smallest anatomical details and ensures precise incisions, especially during minimally invasive or robotic surgeries.
- Personalized Treatment: Data-driven insights allow surgeons to tailor each procedure to the patient’s specific anatomy and health condition.
- Reduced Complications: Predictive algorithms help anticipate bleeding, infection, or anesthesia-related issues, allowing surgeons to act proactively.
- Shorter Recovery Times: Less invasive procedures and improved surgical precision mean faster healing and less post-operative discomfort.
- Better Training for Surgeons: AI-based simulators and feedback tools enhance surgical education and skill development for future professionals.
AI in Urologic and General Surgery
AI is playing an increasingly vital role in urology and general surgery. In urologic procedures, such as prostatectomies or kidney surgeries, AI-guided robotic systems can identify cancerous tissue with remarkable accuracy while preserving healthy structures. Similarly, in general surgery, AI assists in procedures like hernia repairs, gallbladder removals, and colorectal surgeries by improving visualization and precision.
This technology also enables the creation of 3D models of a patient’s anatomy before surgery, allowing for customized surgical strategies that improve efficiency and safety.
Challenges and the Path Forward
While the benefits of artificial intelligence in surgery are clear, there are challenges to consider. Implementing AI systems requires significant investment, strict data privacy measures, and extensive training for medical teams. Additionally, surgeons must maintain human oversight to ensure that decisions remain patient-centered, not purely algorithm-driven.
Despite these hurdles, AI continues to evolve rapidly. As technology becomes more sophisticated and accessible, it’s expected that AI-assisted surgeries will become a standard of care across major medical institutions worldwide.
Experience the Next Generation of Surgical Innovation
The future of surgery is here — driven by artificial intelligence, robotics, and precision medicine. These advancements are helping surgeons perform complex procedures with greater accuracy and safety than ever before.
To learn more about how AI and robotic-assisted techniques can enhance surgical outcomes and recovery, contact our team to schedule a consultation and explore the latest options available for your surgical care.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
What to Expect the Day of Your Surgery
Knowing what to expect on the day of your surgery can help ease anxiety and ensure that everything goes smoothly. For patients undergoing general or minimally invasive procedures, preparation and understanding of the process are key to a safe and successful outcome. Here’s a detailed overview of what typically happens before, during, and after surgery to help you feel informed and confident.

Preparing Before You Arrive
On the day of your surgery, preparation begins long before you step into the operating room. Most patients will receive specific pre-operative instructions from their surgical team in advance. These may include:
- Fasting: You’ll be asked not to eat or drink for a certain number of hours before surgery to prevent complications during anesthesia.
- Medication Adjustments: Some medications may need to be stopped or adjusted prior to surgery, especially blood thinners or diabetes medications.
- Personal Arrangements: Plan to have someone accompany you to and from the hospital or surgical center. You’ll likely be unable to drive afterward.
- Clothing and Belongings: Wear loose, comfortable clothing and leave valuables, jewelry, and makeup at home.
Following these guidelines helps ensure a smoother process once you arrive at the surgical facility.
Check-In and Pre-Operative Preparation
When you arrive, you’ll check in at the surgical reception area. The nursing staff will review your medical history, confirm your procedure, and take vital signs such as blood pressure, temperature, and oxygen levels.
- You’ll change into a hospital gown and remove any personal items.
- An intravenous (IV) line will be placed to administer fluids, medications, and anesthesia.
- You’ll meet with your anesthesiologist, who will explain the anesthesia plan and answer any questions.
- The surgeon may also visit to review final details and mark the surgical site if needed.
This preparation phase is designed to ensure safety and accuracy before entering the operating room.
During the Surgery
Once you’re taken to the operating room, you’ll be connected to monitors that track your heart rate, oxygen levels, and blood pressure throughout the procedure. Depending on the type of surgery, you’ll receive general anesthesia (to make you fully asleep) or regional anesthesia (to numb a specific part of your body).
Your surgical team — which includes the surgeon, anesthesiologist, and nurses — will work together to ensure the highest level of care and precision. For minimally invasive or robotic-assisted procedures, small incisions and advanced technology allow for greater accuracy, less pain, and faster recovery times compared to traditional open surgery.
After the Surgery: Recovery and Monitoring
After the procedure, you’ll be moved to the recovery room, also known as the post-anesthesia care unit (PACU). Here, nurses will monitor your vital signs and ensure you wake comfortably from anesthesia.
- Monitoring: Your blood pressure, pulse, and oxygen will be checked regularly.
- Pain Management: You may receive pain medication through your IV or orally to ensure comfort.
- Observation Time: Most patients remain in recovery for one to two hours before being discharged or moved to a hospital room if an overnight stay is needed.
Your surgeon or a member of the surgical team will discuss the results of your procedure and provide initial recovery instructions.
Post-Surgery Instructions
Before you leave the facility, you’ll receive detailed instructions regarding wound care, activity restrictions, and follow-up appointments. Common guidelines include:
- Keep your incisions clean and dry.
- Avoid heavy lifting or strenuous activity for a few days or weeks.
- Take prescribed medications as directed.
- Contact your doctor immediately if you experience fever, excessive pain, swelling, or bleeding.
Most patients can resume light activities within a few days, especially after minimally invasive procedures. Full recovery times vary depending on the type of surgery and individual healing factors.
Ensuring a Smooth Surgical Experience
The day of surgery can feel overwhelming, but preparation and communication make a major difference. Arriving early, following pre-op instructions, and asking questions about your recovery plan all help create a positive and safe experience. Modern surgical techniques and attentive post-operative care are designed to minimize discomfort and promote faster healing.
If you’re scheduled for surgery or planning one soon, our experienced surgical team is here to guide you through every step — from preparation to recovery. Reach out today to schedule a consultation or to learn more about what to expect for your procedure.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Gallbladder Problems: Signs You Shouldn’t Ignore
Gallbladder problems can cause a range of symptoms that may start subtly but can quickly become severe if left untreated. Recognizing the early signs of gallbladder disease is essential for preventing complications and maintaining digestive health. Common conditions that affect the gallbladder include gallstones, inflammation (cholecystitis), and bile duct obstruction. Understanding these warning signs can help you seek timely medical care and avoid unnecessary discomfort.
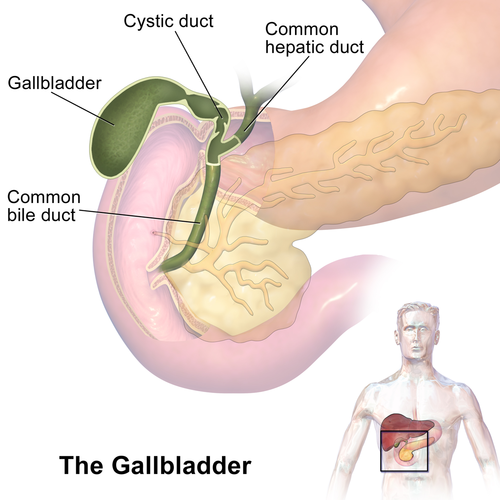
Understanding the Role of the Gallbladder
The gallbladder is a small, pear-shaped organ located beneath the liver. Its main function is to store and release bile — a digestive fluid produced by the liver that helps break down fats. When the gallbladder becomes inflamed, blocked, or infected, it can cause pain and interfere with normal digestion.
Common Signs of Gallbladder Problems
Gallbladder issues often manifest through specific symptoms. While they may resemble other digestive disorders, these warning signs typically indicate the need for medical evaluation:
- Abdominal Pain: Sharp or cramping pain in the upper right abdomen is one of the most common symptoms. The pain may radiate to the back or right shoulder and often worsens after eating fatty foods.
- Nausea and Vomiting: Persistent nausea, especially after meals, can suggest bile flow disruption caused by gallstones or inflammation.
- Indigestion and Bloating: Frequent bloating, gas, or discomfort after eating can be signs that your gallbladder is not functioning properly.
- Fever or Chills: A fever accompanied by abdominal pain could indicate infection, such as acute cholecystitis, which requires immediate attention.
- Changes in Stool or Urine Color: Pale stools or dark urine may point to bile duct obstruction, which can prevent bile from reaching the intestines.
- Jaundice: Yellowing of the skin or eyes suggests bile buildup due to a blockage and requires urgent evaluation.
What Causes Gallbladder Disease?
Gallbladder problems are most commonly linked to gallstones — hardened deposits of digestive fluid that can block bile ducts. Risk factors for gallstones include:
- Obesity or rapid weight loss
- High-fat or high-cholesterol diet
- Female gender and age over 40
- Family history of gallstones
- Pregnancy or hormonal therapy
Other causes include bile duct strictures, infection, or poor gallbladder function due to chronic inflammation.
When to Seek Medical Attention
You should not ignore persistent or severe abdominal pain, especially if it is accompanied by nausea, fever, or jaundice. These symptoms could indicate a serious gallbladder issue requiring prompt medical evaluation. In some cases, untreated gallbladder disease can lead to life-threatening infections or the rupture of the gallbladder.
Treatment Options for Gallbladder Problems
The appropriate treatment depends on the severity of the condition and underlying cause. Common treatment options include:
- Medication: For mild inflammation or to dissolve small gallstones, certain medications may be prescribed.
- Dietary Adjustments: Reducing fatty and greasy foods can help manage symptoms and prevent further irritation.
- Minimally Invasive Surgery: Laparoscopic or robotic-assisted cholecystectomy (gallbladder removal) is often the most effective and permanent treatment for recurrent or severe gallbladder problems.
Modern minimally invasive techniques offer shorter recovery times, smaller scars, and less post-operative pain compared to traditional open surgery.
Protecting Your Gallbladder Health
Maintaining a healthy lifestyle is key to preventing gallbladder issues. Consider these preventive measures:
- Eat a balanced diet rich in fiber and low in saturated fats.
- Stay physically active to support healthy digestion.
- Maintain a stable weight — avoid rapid weight loss or crash diets.
- Stay hydrated to promote optimal bile consistency.
Even if you are not experiencing symptoms, routine medical checkups can help detect gallbladder issues early and prevent complications.
Get Expert Care for Gallbladder Problems
If you’re experiencing symptoms of gallbladder disease or suspect you have gallstones, it’s important to seek professional medical evaluation. Advanced diagnostic imaging and minimally invasive surgical options can effectively resolve most gallbladder issues while minimizing recovery time.
Contact our team today to schedule a consultation and discuss the best treatment plan for your health needs.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Robotic Surgery Vs. Traditional Laparoscopy
 Robotic surgery has transformed the field of minimally invasive surgery, providing enhanced precision, flexibility, and control compared to traditional laparoscopy. For patients in New York City, understanding how robotic surgery differs from standard laparoscopic procedures can help them make informed decisions about their care.
Robotic surgery has transformed the field of minimally invasive surgery, providing enhanced precision, flexibility, and control compared to traditional laparoscopy. For patients in New York City, understanding how robotic surgery differs from standard laparoscopic procedures can help them make informed decisions about their care.
At Lenox Hill Surgeons, Dr. Roman Grinberg specializes in advanced robotic-assisted urologic surgery, offering patients innovative treatment options for conditions affecting the prostate, bladder, and kidneys.
How Traditional Laparoscopy Works
Traditional laparoscopic surgery is a minimally invasive technique that uses small incisions, a camera (laparoscope), and specialized instruments to perform surgical procedures. Surgeons view the surgical area on a 2D monitor while manually controlling the instruments.
- Smaller incisions reduce pain and scarring.
- Shorter hospital stays and recovery times compared to open surgery.
- Limited range of motion for instruments and dependence on 2D visualization.
While laparoscopic surgery revolutionized modern surgery by minimizing trauma to the body, it still presents challenges when precision and dexterity are critical — especially in delicate urological procedures.
The Advantages of Robotic Surgery
Robotic surgery builds upon the foundations of laparoscopy but incorporates state-of-the-art technology to enhance the surgeon’s capabilities. Using systems like the da Vinci® Surgical System, Dr. Grinberg controls robotic arms from a console equipped with 3D high-definition visualization and wristed instruments that mimic the movement of the human hand.
Key advantages of robotic surgery include:
- Enhanced Precision: Robotic instruments filter out hand tremors, allowing for micro-movements that are impossible with human hands.
- Better Visualization: The 3D high-definition camera provides a magnified, immersive view of the surgical field.
- Improved Range of Motion: Wristed instruments move with greater dexterity than traditional laparoscopic tools.
- Minimized Blood Loss and Scarring: Smaller incisions and refined control reduce tissue trauma.
- Faster Recovery: Most patients experience less post-operative pain and quicker return to normal activities.
Applications in Urologic Surgery
Dr. Roman Grinberg utilizes robotic surgery for a wide range of urological procedures, including:
- Robotic prostatectomy for prostate cancer
- Partial nephrectomy for kidney tumors
- Bladder reconstruction and diverticulectomy
- Ureteral reimplantation and other complex reconstructive surgeries
These procedures benefit significantly from the precision and accuracy that robotic assistance provides, leading to improved surgical outcomes and reduced complications.
Why Choose Robotic Surgery in NYC?
Patients in New York City benefit from access to cutting-edge surgical technology and highly skilled specialists like Dr. Grinberg. Robotic surgery allows for greater surgical accuracy in a minimally invasive setting — an essential advantage in treating sensitive organs of the urinary system.
Moreover, the patient experience is enhanced by shorter hospital stays, faster recovery, and reduced post-operative discomfort. These advantages make robotic-assisted surgery an increasingly preferred choice for both surgeons and patients.
Experience the Future of Surgical Precision with Dr. Grinberg
If you’re considering minimally invasive treatment for a urological condition, schedule a consultation with Dr. Roman Grinberg at Lenox Hill Surgeons. Discover how robotic-assisted surgery can provide safer, faster, and more precise results tailored to your needs. Call today to learn more or to book your appointment.
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
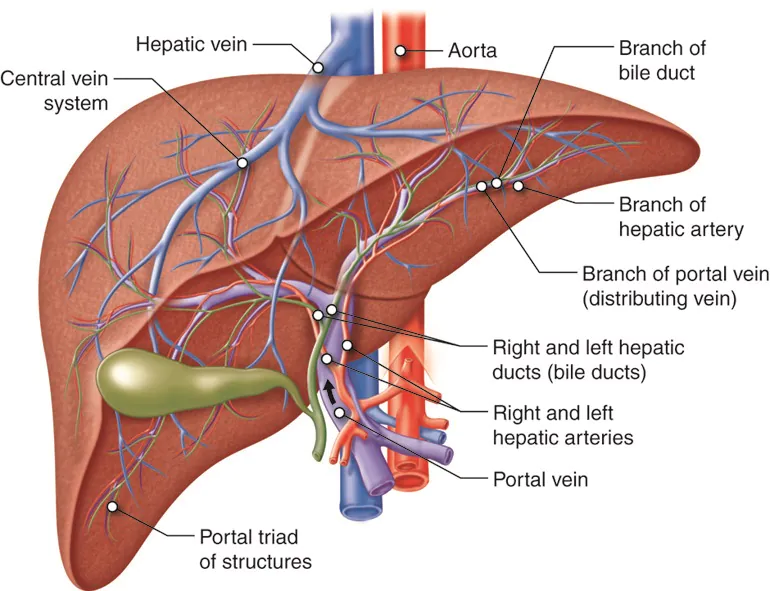
Liver Surgery: What Patients Need to Know About Resection and Transplantation
The liver is one of the most vital organs in the body, responsible for detoxification, metabolism, and digestion. When diseases such as liver cancer, cirrhosis, or severe liver injury impair its function, surgical intervention may be necessary. Liver surgery typically involves resection (partial removal of the liver) or, in severe cases, a liver transplant.
This guide will explain when liver surgery is needed, the differences between liver resection and transplantation, and what patients can expect during recovery.
When Is Liver Surgery Necessary?
Liver surgery is typically required for patients with tumors, liver failure, or irreversible damage. Some of the most common conditions that may require surgery include:
- Liver Cancer (Hepatocellular Carcinoma): Malignant tumors that originate in the liver.
- Metastatic Liver Cancer: Cancer that has spread to the liver from another part of the body.
- Benign Liver Tumors: Noncancerous growths that may require removal if they cause symptoms.
- Cirrhosis: Severe scarring of the liver, often caused by alcohol abuse or viral hepatitis.
- Liver Cysts and Abscesses: Fluid-filled sacs or infections that require drainage or removal.
- Liver Trauma: Severe injury to the liver due to accidents or blunt force trauma.
- End-Stage Liver Disease: When liver failure becomes life-threatening, a liver transplant may be necessary.
Types of Liver Surgery
There are two primary types of liver surgery: liver resection (partial hepatectomy) and liver transplantation. The best surgical option depends on the underlying condition, liver function, and overall patient health.
1. Liver Resection (Partial Hepatectomy)
Liver resection, also known as partial hepatectomy, involves removing a portion of the liver affected by tumors, cysts, or damaged tissue while preserving the remaining healthy liver.
When Is Liver Resection Needed?
Liver resection is commonly performed for:
- Primary Liver Cancer (Hepatocellular Carcinoma): If the tumor is localized and the rest of the liver is healthy.
- Metastatic Liver Cancer: To remove cancer that has spread from another organ.
- Benign Tumors and Cysts: If they are large or causing symptoms.
How the Procedure Works:
- Surgeons make an incision in the abdomen to access the liver.
- The diseased portion of the liver is carefully removed.
- The remaining liver is left intact and continues to function.
- The liver has a remarkable ability to regenerate, often regrowing within a few months.
Benefits of Liver Resection:
- Preserves a functioning portion of the liver.
- Can completely remove localized tumors.
- Less invasive than a full liver transplant.
Potential Risks:
- Risk of bleeding, since the liver contains many blood vessels.
- Possible infection or complications from anesthesia.
- May not be an option for patients with severe cirrhosis or liver failure.
2. Liver Transplantation
A liver transplant is a procedure in which a diseased liver is completely removed and replaced with a healthy liver from a donor. This is typically the last resort for patients with end-stage liver disease or irreversible liver failure.
When Is a Liver Transplant Needed?
Liver transplantation is recommended for patients with:
- End-Stage Liver Disease: Severe liver damage due to cirrhosis or chronic hepatitis.
- Acute Liver Failure: Sudden loss of liver function, often due to poisoning or viral infections.
- Liver Cancer: If cancer is confined to the liver but cannot be removed with resection.
Types of Liver Transplants:
- Deceased Donor Liver Transplant: The entire liver is obtained from a deceased donor.
- Living Donor Liver Transplant: A portion of a healthy person’s liver is transplanted, and both donor and recipient’s livers regenerate over time.
How the Procedure Works:
- The diseased liver is removed completely.
- The donor liver (or liver portion) is placed in its position.
- Surgeons connect the blood vessels and bile ducts to restore normal function.
- Patients require lifelong immunosuppressive medications to prevent organ rejection.
Benefits of Liver Transplantation:
- Can completely cure end-stage liver disease.
- Provides a long-term solution for patients with severe liver failure.
Potential Risks:
- Long waiting times for donor livers.
- Risk of organ rejection, requiring lifelong immunosuppressants.
- Increased risk of infections and complications post-surgery.
Recovery After Liver Surgery
The recovery process depends on the type of liver surgery performed. Liver resection typically requires a shorter recovery than a full liver transplant.
What to Expect After Liver Resection:
- Hospital stay: 5-7 days.
- Return to normal activities: 4-8 weeks.
- Pain and discomfort managed with medication.
- Follow-up scans to monitor liver regeneration.
What to Expect After a Liver Transplant:
- Hospital stay: 2-3 weeks.
- Recovery period: 3-6 months.
- Lifelong immunosuppressive medications to prevent rejection.
- Frequent follow-up appointments and blood tests.
Long-Term Outlook After Liver Surgery
Most patients who undergo liver resection recover well if the remaining liver is healthy. Those who receive liver transplants can live long, fulfilling lives, but they must carefully manage their health to prevent complications.
How to Maintain Liver Health After Surgery
- Eat a balanced diet rich in fruits, vegetables, and lean proteins.
- Avoid alcohol and toxic substances that can damage the liver.
- Exercise regularly to maintain a healthy weight.
- Take prescribed medications as directed by your doctor.
- Attend all follow-up appointments and screenings.
Conclusion: Choosing the Right Liver Surgery for Your Condition
Liver surgery, whether resection or transplantation, can be a life-saving procedure for individuals with liver disease. Liver resection is often used for localized tumors, while liver transplants are the best option for end-stage liver failure. Advances in surgical techniques and post-operative care have greatly improved patient outcomes, offering long-term survival and improved quality of life.
If you or a loved one is facing liver disease and considering surgery, the expert team at Lenox Hill Surgeons is here to help. Our skilled surgeons specialize in advanced liver surgery techniques, providing personalized care and the best possible outcomes.
Schedule a consultation today to discuss your options.
Contact Information
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Esophageal Surgery for GERD and Acid Reflux: Surgical Options for Long-Term Relief
Is esophageal surgery required for GERD? Gastroesophageal reflux disease (GERD) is a chronic digestive condition where stomach acid flows back into the esophagus, causing heartburn, regurgitation, and irritation. While lifestyle changes and medications can manage GERD for many people, some individuals experience severe or persistent symptoms that require surgical intervention. Esophageal surgery offers a long-term solution for patients who do not respond to other treatments.
This guide explores when surgery is necessary for GERD, the different surgical options available, and what patients can expect during recovery.

Understanding GERD and Acid Reflux
GERD occurs when the lower esophageal sphincter (LES)—the muscle that separates the esophagus from the stomach—becomes weak or dysfunctional, allowing stomach acid to flow back up into the esophagus.
Common Symptoms of GERD
- Frequent heartburn (burning sensation in the chest)
- Acid regurgitation (sour taste in the mouth)
- Difficulty swallowing (dysphagia)
- Chronic cough or hoarseness
- Feeling of food stuck in the throat
- Chest pain (often mistaken for heart-related issues)
If GERD is left untreated, it can lead to serious complications, including esophagitis (inflammation of the esophagus), Barrett’s esophagus (precancerous condition), and esophageal strictures (narrowing of the esophagus).
When Is Esophageal Surgery Needed for GERD?
While antacids, proton pump inhibitors (PPIs), and dietary modifications help many people manage GERD, surgery may be necessary if:
- Medications are ineffective or require lifelong use
- Symptoms severely impact quality of life
- Esophageal damage (such as ulcers or strictures) is present
- Complications such as Barrett’s esophagus develop
- Chronic reflux leads to aspiration pneumonia or respiratory issues
For patients who suffer from severe acid reflux, surgical procedures provide long-term relief by addressing the root cause of GERD.
Surgical Treatment Options for GERD
There are several surgical procedures available for treating chronic acid reflux and GERD. The most appropriate option depends on the patient’s condition, severity of symptoms, and overall health.
1. Laparoscopic Nissen Fundoplication
Nissen fundoplication is the gold standard for GERD surgery. This procedure reinforces the lower esophageal sphincter (LES) to prevent acid reflux.
How It Works:
- The upper portion of the stomach (fundus) is wrapped around the lower esophagus
- This strengthens the LES and prevents stomach acid from flowing backward
- Performed laparoscopically (minimally invasive), reducing recovery time
Benefits of Nissen Fundoplication:
- High success rate for long-term GERD relief
- Minimally invasive with small incisions
- Most patients can discontinue acid reflux medications
2. LINX® Reflux Management System
The LINX® system is a minimally invasive implantable device used to treat GERD.
How It Works:
- A small magnetic ring is placed around the LES
- The device reinforces the LES while still allowing normal swallowing
- It prevents acid reflux while maintaining natural function
Benefits of LINX Surgery:
- Quick outpatient procedure (often same-day discharge)
- Shorter recovery time compared to fundoplication
- Preserves the ability to burp and vomit, unlike fundoplication
3. Transoral Incisionless Fundoplication (TIF)
TIF is an advanced endoscopic procedure for GERD that does not require incisions.
How It Works:
- A flexible endoscope is inserted through the mouth
- The top of the stomach is folded around the LES to strengthen it
- The procedure is done without external cuts
Benefits of TIF Surgery:
- Completely incision-free
- Faster recovery and minimal post-surgical pain
- Effective for mild to moderate GERD cases
4. Hiatal Hernia Repair
A hiatal hernia occurs when the stomach pushes through the diaphragm, worsening GERD symptoms. In some cases, hiatal hernia repair is necessary along with fundoplication.
How It Works:
- The hernia is repositioned into the abdomen
- The diaphragm opening is tightened to prevent further displacement
- This repair reduces reflux and improves LES function
Benefits of Hiatal Hernia Repair:
- Addresses the root cause of GERD in patients with a hernia
- Minimally invasive with laparoscopic techniques
- Long-term acid reflux relief
What to Expect After GERD Surgery
Recovery after esophageal surgery varies depending on the procedure. Most minimally invasive GERD surgeries allow patients to return home the same day or within 24 hours.
Post-Surgical Recovery Timeline
- Hospital Stay: 1-2 days for fundoplication; same-day discharge for LINX or TIF
- Pain Management: Minimal discomfort managed with mild pain medications
- Dietary Changes: Liquid or soft food diet for 1-2 weeks
- Activity Restrictions: Avoid strenuous activities for 2-4 weeks
Potential Side Effects
While GERD surgery is safe and effective, some patients may experience:
- Difficulty swallowing (temporary after fundoplication)
- Increased gas or bloating
- Changes in burping or vomiting ability
Most side effects improve within a few weeks after surgery.
Choosing the Best GERD Surgery for You
The right surgical option depends on the severity of GERD, presence of a hiatal hernia, and overall health.
- Best for severe GERD: Nissen fundoplication
- Best for mild to moderate GERD: TIF or LINX system
- Best for GERD with a hiatal hernia: Hiatal hernia repair + fundoplication
A gastroenterologist and general surgeon can help determine the best approach for long-term acid reflux relief.
Conclusion: Regain Control Over GERD with Advanced Surgical Care
If GERD is interfering with your daily life, and medications are no longer effective, esophageal surgery may be the solution for long-term relief. Minimally invasive procedures, such as laparoscopic fundoplication, LINX, and TIF, provide lasting results with minimal recovery time.
If you’re suffering from chronic acid reflux, don’t wait—seek expert care today. At Lenox Hill Surgeons, we specialize in advanced GERD surgical treatments tailored to your needs. Schedule a consultation to explore your options and take the first step toward a reflux-free life.
Contact Information
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Minimally Invasive Surgery: The Benefits of Laparoscopic and Robotic Procedures
 Surgical advancements have transformed the way medical professionals treat a wide range of conditions. Minimally invasive surgery (MIS) has become the preferred approach for many procedures, offering reduced pain, shorter recovery times, and fewer complications compared to traditional open surgery. Two of the most widely used minimally invasive techniques are laparoscopic surgery and robotic-assisted surgery, both of which allow surgeons to perform complex procedures with greater precision and control.
Surgical advancements have transformed the way medical professionals treat a wide range of conditions. Minimally invasive surgery (MIS) has become the preferred approach for many procedures, offering reduced pain, shorter recovery times, and fewer complications compared to traditional open surgery. Two of the most widely used minimally invasive techniques are laparoscopic surgery and robotic-assisted surgery, both of which allow surgeons to perform complex procedures with greater precision and control.
This guide explores the benefits of minimally invasive surgery, the differences between laparoscopic and robotic procedures, and the conditions that can be treated using these advanced surgical techniques.
What Is Minimally Invasive Surgery?
Minimally invasive surgery involves small incisions, specialized instruments, and high-tech imaging to perform surgical procedures with minimal trauma to the body. Instead of making a large incision, surgeons use tiny cameras and precision tools to operate with enhanced accuracy.
Key Advantages of Minimally Invasive Surgery
- Smaller incisions result in minimal scarring
- Reduced pain and discomfort post-surgery
- Shorter hospital stays (often same-day discharge)
- Faster recovery time, allowing patients to resume daily activities sooner
- Lower risk of infection and post-operative complications
- Less blood loss, reducing the need for transfusions
Minimally invasive techniques are particularly useful for general surgery, gastrointestinal procedures, and gynecological and urological surgeries.
Laparoscopic Surgery: A Minimally Invasive Standard
Laparoscopic surgery is one of the most commonly used minimally invasive techniques. It involves making small incisions, through which a laparoscope (a thin tube with a camera) and specialized instruments are inserted to perform the procedure.
How Laparoscopic Surgery Works
- A small incision is made near the surgical site
- A laparoscope (a small camera) is inserted to provide a clear view of the internal structures
- Surgeons use long, thin instruments to complete the surgery with precision
- The incisions are closed with minimal sutures
Benefits of Laparoscopic Surgery
- Minimally invasive approach reduces trauma to surrounding tissues
- Less post-operative pain compared to open surgery
- Faster healing and shorter recovery time
- Lower risk of complications, such as infections and blood clots
Common Procedures Performed Using Laparoscopic Surgery
Laparoscopic techniques are widely used in various surgical specialties, including:
- Gallbladder removal (cholecystectomy): A standard treatment for gallstones and gallbladder disease
- Hernia repair: Used to reinforce weakened abdominal walls
- Appendectomy: A minimally invasive option for treating appendicitis
- Colorectal surgery: Used for the treatment of diverticulitis, colorectal cancer, and inflammatory bowel disease
- Gastroesophageal reflux disease (GERD) surgery: A laparoscopic fundoplication can help manage severe acid reflux
Robotic-Assisted Surgery: Enhancing Precision and Control
 Robotic-assisted surgery is an advanced form of minimally invasive surgery that provides greater precision, flexibility, and control. The da Vinci Surgical System is the most commonly used robotic surgical platform, allowing surgeons to perform complex procedures with improved dexterity.
Robotic-assisted surgery is an advanced form of minimally invasive surgery that provides greater precision, flexibility, and control. The da Vinci Surgical System is the most commonly used robotic surgical platform, allowing surgeons to perform complex procedures with improved dexterity.
How Robotic-Assisted Surgery Works
Unlike traditional laparoscopy, robotic surgery involves:
- Surgeon-controlled robotic arms, which replicate natural hand movements with extreme precision
- High-definition 3D imaging, providing a magnified view of the surgical site
- Enhanced range of motion, allowing for delicate and intricate surgical maneuvers
Benefits of Robotic Surgery
Robotic-assisted procedures provide greater accuracy and better patient outcomes, especially for complex or delicate surgeries.
- Increased precision and control: The robotic system eliminates natural hand tremors, allowing for steady, precise movements
- Smaller incisions and minimal scarring
- Less blood loss and faster recovery times
- Improved visualization: Surgeons see a 3D, high-resolution image of the surgical area
- Better outcomes for delicate procedures, such as prostate surgery and colorectal resections
Common Procedures Performed Using Robotic Surgery
Robotic-assisted surgery is commonly used in:
- Hernia repairs: Provides greater precision for complex hernias
- Colorectal surgery: Used for colon cancer, diverticulitis, and inflammatory bowel disease
- Prostate surgery: Often the preferred method for prostatectomy (removal of the prostate gland)
- Gynecological procedures: Such as hysterectomy and myomectomy
- Thoracic surgery: Used for lung cancer and esophageal surgeries
Comparing Laparoscopic vs. Robotic Surgery
While both techniques offer minimally invasive benefits, there are key differences.
| Feature | Laparoscopic Surgery | Robotic-Assisted Surgery |
|---|---|---|
| Incision Size | Small (5-10mm) | Small (5-10mm) |
| Visualization | 2D HD Camera | 3D High-Definition Imaging |
| Surgeon Control | Hand-operated instruments | Robotic arms controlled by surgeon |
| Best For | Routine minimally invasive procedures | Complex or delicate surgeries requiring enhanced precision |
Recovery After Minimally Invasive Surgery
Minimally invasive procedures allow for quicker recovery times than traditional open surgery.
What to Expect Post-Surgery
- Hospital Stay: Most patients return home the same day or within 24 hours
- Pain Management: Over-the-counter or mild prescription pain medications
- Activity Restrictions: Avoid heavy lifting and strenuous exercise for 2-4 weeks
- Return to Normal Activities: Within 1-2 weeks for laparoscopic surgery and 2-3 weeks for robotic surgery
Conclusion: Choosing the Right Minimally Invasive Surgery
Minimally invasive surgical techniques, including laparoscopic and robotic-assisted surgery, provide safer, faster, and more effective options for a variety of medical conditions. Whether undergoing hernia repair, gallbladder surgery, or colorectal procedures, these advanced techniques allow for faster recovery, less pain, and improved surgical outcomes.
If you are considering surgery and want to explore minimally invasive options, our expert team at Lenox Hill Surgeons specializes in advanced laparoscopic and robotic-assisted procedures. Contact us today to discuss the best surgical approach for your condition and experience world-class surgical care.
Contact Information
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Appendix Surgery: Understanding Appendicitis and Emergency Surgical Care
What is appendicitis and at what point is emergency surgical care necessary? The appendix is a small, tube-like organ located in the lower right abdomen. While its exact function is not entirely understood, it can become inflamed or infected, leading to a condition known as appendicitis. If left untreated, appendicitis can lead to serious complications, including rupture (perforation) and widespread infection. In most cases, the best and safest treatment is an appendectomy, or surgical removal of the appendix.
This guide will cover the causes, symptoms, and treatment options for appendicitis, when emergency surgery is necessary, and what patients can expect during recovery.

What Is Appendicitis?
Appendicitis occurs when the appendix becomes blocked, inflamed, and filled with pus. This blockage may result from:
- Hardened stool (fecalith): A solid mass that obstructs the appendix
- Infection: A bacterial or viral infection that triggers swelling
- Enlarged lymph tissue: Inflammation from other infections in the body
- Foreign objects: Rare cases where seeds or other materials block the appendix
Without prompt medical attention, the appendix can rupture, spreading infection throughout the abdomen (peritonitis) or forming an abscess.
Recognizing the Symptoms of Appendicitis
Appendicitis typically starts with mild pain that worsens over time. Symptoms include:
- Severe abdominal pain: Often begins near the navel and moves to the lower right side of the abdomen
- Loss of appetite: A common early symptom
- Nausea and vomiting: Often follows the onset of pain
- Fever and chills: May indicate infection
- Swelling in the abdomen: A sign of worsening inflammation
- Difficulty passing gas or stool: May indicate a blockage
- Increased pain with movement: Walking or coughing may worsen pain
When to Seek Emergency Medical Care
Appendicitis is a medical emergency. If you experience severe pain, fever, or worsening symptoms, seek immediate medical attention. A ruptured appendix can lead to life-threatening infections and requires urgent surgical intervention.
How Is Appendicitis Diagnosed?
Doctors use several diagnostic tools to confirm appendicitis, including:
- Physical Exam: Checking for tenderness in the lower right abdomen
- Blood Tests: Detecting elevated white blood cell count, indicating infection
- Imaging Tests: Ultrasound, CT scans, or MRI to visualize inflammation or rupture
Surgical Treatment: Appendectomy
An appendectomy is the standard treatment for appendicitis. It is a safe and effective procedure that prevents complications and eliminates the risk of recurrence.
Types of Appendectomy
There are two main surgical approaches to removing the appendix:
1. Laparoscopic Appendectomy (Minimally Invasive Surgery)
A laparoscopic appendectomy is the preferred method when appendicitis is caught early. This technique involves:
- Small incisions in the abdomen
- Insertion of a laparoscope (a tiny camera) for precise removal
- Minimal scarring and a quicker recovery
Advantages:
- Less post-operative pain
- Shorter hospital stay (often same-day discharge)
- Lower risk of infection
- Faster return to normal activities (within 1-2 weeks)
2. Open Appendectomy
An open appendectomy is performed when the appendix has ruptured or if severe infection is present. This procedure involves:
- A single, larger incision in the lower right abdomen
- Manual removal of the appendix
- Cleaning of any infection or abscess
Advantages:
- More effective for complicated cases, including ruptured appendix
Disadvantages:
- Longer recovery (typically 4-6 weeks)
- Higher risk of infection due to potential contamination
What to Expect After Appendectomy
Recovery time depends on the type of surgery and whether complications occurred.
Post-Surgical Recovery Timeline
- Hospital Stay: Same-day discharge for laparoscopic surgery; 1-3 days for open surgery
- Pain Management: Mild pain is common, managed with over-the-counter or prescribed medication
- Activity Restrictions: Avoid heavy lifting and strenuous exercise for 2-4 weeks
- Diet: Start with a soft diet, then gradually reintroduce solid foods
- Follow-Up Appointment: Usually scheduled 1-2 weeks after surgery
When to Contact Your Doctor
While most patients recover without complications, contact your doctor if you experience:
- Persistent fever over 101°F (38.3°C)
- Increasing abdominal pain
- Redness, swelling, or pus around the incision site
- Difficulty urinating or severe bloating
- Persistent nausea or vomiting
Can You Live Without an Appendix?
Yes! The appendix does not serve a critical function in adults, and people live healthy, normal lives after its removal. There are no major dietary or lifestyle restrictions following an appendectomy, though maintaining a balanced diet and staying hydrated helps support overall digestive health.
Preventing Appendicitis
While there is no guaranteed way to prevent appendicitis, maintaining a healthy digestive system may help reduce risk. Some key strategies include:
- Eating a high-fiber diet (fruits, vegetables, whole grains)
- Staying well-hydrated
- Managing gut health with probiotics and fermented foods
- Seeking medical attention for persistent digestive discomfort
Conclusion: When to Consider Surgery for Appendicitis
Appendicitis is a medical emergency that requires immediate attention. If you experience severe abdominal pain, nausea, fever, or signs of a ruptured appendix, seeking emergency care is critical. Surgical removal of the appendix (appendectomy) is a safe and effective procedure that prevents life-threatening complications and promotes long-term health.
If you or a loved one is experiencing symptoms of appendicitis, don’t wait—early diagnosis and prompt surgical intervention lead to the best outcomes. The expert surgeons at Lenox Hill Surgeons specialize in minimally invasive and emergency appendectomies, ensuring the highest level of care. Contact us today for expert surgical consultation and treatment.
Contact Information
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Gallbladder Surgery: When Is Cholecystectomy the Right Choice?
This guide will help you understand when gallbladder surgery is necessary, the different types of cholecystectomy, and what to expect during recovery. The gallbladder is a small organ located beneath the liver that plays an essential role in digestion by storing and releasing bile. However, when the gallbladder develops gallstones, inflammation, or other complications, it can lead to significant pain and digestive issues. In many cases, a cholecystectomy—the surgical removal of the gallbladder—is the most effective treatment.
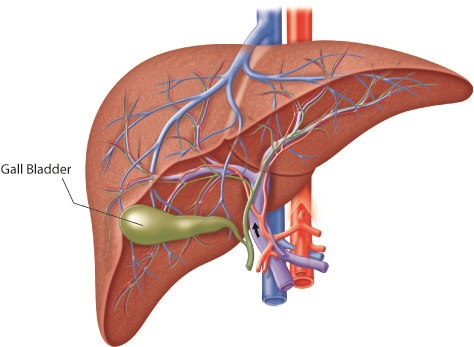
Understanding Gallbladder Problems
The gallbladder helps break down fats by releasing bile into the small intestine. However, certain conditions can interfere with its function, causing pain and discomfort.
Common Gallbladder Conditions That May Require Surgery
- Gallstones (Cholelithiasis): Hardened deposits of bile that can block the bile ducts and cause pain.
- Gallbladder Inflammation (Cholecystitis): Inflammation due to infection or gallstone obstruction, leading to severe pain and fever.
- Biliary Dyskinesia: A condition in which the gallbladder doesn’t empty bile properly, causing chronic digestive symptoms.
- Gallbladder Polyps: Growths in the gallbladder that, if large, may increase the risk of cancer.
- Gallbladder Cancer: A rare but serious condition where tumor growth may necessitate gallbladder removal.
When Is Gallbladder Surgery Necessary?
Not all gallbladder issues require surgery. However, a cholecystectomy is often recommended when symptoms become severe or when complications arise.
Signs That You May Need Gallbladder Surgery
- Severe and recurring abdominal pain, especially in the upper right side
- Nausea and vomiting after meals
- Frequent bloating and indigestion
- Jaundice (yellowing of the skin and eyes), indicating bile duct blockage
- High fever and chills, suggesting infection
If gallstones or inflammation are causing persistent pain or interfering with digestion, removing the gallbladder is often the best treatment.
Types of Gallbladder Surgery
There are two main types of cholecystectomy procedures: laparoscopic (minimally invasive) surgery and open surgery. The choice depends on the severity of the condition and the patient’s medical history.
1. Laparoscopic Cholecystectomy (Minimally Invasive Surgery)
Laparoscopic cholecystectomy is the most common and preferred method for gallbladder removal. It involves small incisions and the use of a tiny camera (laparoscope) to guide the surgery.
Advantages:
- Smaller incisions and minimal scarring
- Less post-operative pain
- Shorter hospital stay (often same-day discharge)
- Faster recovery (most patients resume normal activities within a week)
Disadvantages:
- Not suitable for all cases, especially if severe inflammation or complications exist
2. Open Cholecystectomy
An open cholecystectomy is performed when laparoscopic surgery is not an option, such as when there is severe infection, scarring from previous surgeries, or complications like a ruptured gallbladder.
Advantages:
- More effective for complicated gallbladder conditions
- Better visualization for the surgeon in cases of extensive scarring
Disadvantages:
- Larger incision and more scarring
- Longer hospital stay (usually 2-4 days)
- Longer recovery period (4-6 weeks)
What to Expect During Gallbladder Surgery
Regardless of the technique used, a cholecystectomy is a routine and safe procedure. Here’s what patients can expect before, during, and after surgery.
Pre-Surgical Preparation
- Fasting for at least 8 hours before surgery
- Stopping certain medications that may increase bleeding risk
- Preoperative tests such as blood work and imaging scans
During the Procedure
- Performed under general anesthesia
- Incisions made in the abdomen (either small for laparoscopic surgery or a larger one for open surgery)
- Removal of the gallbladder, followed by closure of the incisions
The procedure typically takes 1-2 hours, and most laparoscopic patients can go home the same day.
Post-Surgical Recovery
Recovery depends on the type of surgery performed.
- Laparoscopic Surgery: Most patients can return to normal activities within one week.
- Open Surgery: Full recovery may take 4-6 weeks due to the larger incision.
Tips for a Smooth Recovery:
- Follow a low-fat diet initially to help digestion adjust
- Drink plenty of water and eat fiber-rich foods to prevent constipation
- Avoid heavy lifting or strenuous activities for at least two weeks
- Monitor for signs of infection such as redness, swelling, or fever
Life Without a Gallbladder
The gallbladder is not an essential organ, and most people live completely normal lives after its removal. However, some individuals may experience temporary digestive changes, including:
- More frequent bowel movements
- Mild bloating or gas
- Difficulty digesting high-fat foods
Most digestive issues improve over time, and dietary adjustments can help ease the transition.
When to Seek Emergency Care
While gallbladder surgery is generally safe, complications can arise. Seek medical attention if you experience:
- Severe or worsening abdominal pain
- Persistent nausea or vomiting
- High fever or chills
- Yellowing of the skin or eyes (jaundice)
- Swelling, redness, or discharge from the incision site
Conclusion: Is Gallbladder Surgery Right for You?
If you suffer from chronic gallbladder pain, gallstones, or recurrent inflammation, cholecystectomy may be the best option for long-term relief. Minimally invasive laparoscopic surgery offers a quick and effective solution with minimal downtime, while open surgery is reserved for more complex cases.
Consulting a qualified general surgeon is the first step in determining whether gallbladder surgery is right for you. If you’re struggling with persistent gallbladder symptoms, don’t wait—early intervention can prevent complications and improve your quality of life.
If you’re considering gallbladder surgery, the expert team at Lenox Hill Surgeons is here to help. Our experienced surgeons specialize in minimally invasive and advanced gallbladder procedures to ensure the best possible outcomes.
Schedule a consultation today and take the first step toward relief.
Contact Information
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Hernia Repair Surgery: Types, Symptoms, and the Best Treatment Options
This blog is about hernia repair surgery. A hernia occurs when an organ or tissue pushes through a weak spot in the surrounding muscle or connective tissue, often leading to discomfort, pain, and potential complications if left untreated. While some hernias may be managed with lifestyle adjustments, surgery remains the most effective long-term solution to repair the weakened area and prevent recurrence.
This guide explores the different types of hernias, common symptoms, and the best treatment options available, including minimally invasive surgical techniques that promote faster recovery.

Understanding Different Types of Hernias
Hernias can develop in different parts of the body, but the most common types occur in the abdominal and groin areas.
1. Inguinal Hernia
An inguinal hernia is the most common type, occurring when a portion of the intestine or fatty tissue pushes through the abdominal wall near the groin area. This type of hernia is more common in men.
Symptoms:
- A visible bulge in the groin or scrotum
- Pain or discomfort, especially when lifting or coughing
- Weakness or pressure in the groin area
- Burning or aching sensation at the site of the hernia
2. Umbilical Hernia
An umbilical hernia occurs when part of the intestine pushes through the abdominal wall near the belly button. It is common in infants but can also affect adults, especially those who are overweight or have had multiple pregnancies.
Symptoms:
- Swelling or bulging around the belly button
- Discomfort or pain when pressing on the area
- Increased swelling when standing or straining
3. Hiatal Hernia
A hiatal hernia occurs when part of the stomach pushes through the diaphragm into the chest cavity. This type of hernia is associated with acid reflux and GERD (gastroesophageal reflux disease).
Symptoms:
- Heartburn and acid reflux
- Difficulty swallowing
- Chest pain or discomfort
- Regurgitation of food or sour liquid
4. Incisional Hernia
An incisional hernia can develop at the site of a previous surgical incision, where the abdominal wall has weakened. This is more common in individuals who have had major abdominal surgeries.
Symptoms:
- Bulging or swelling near a previous surgical scar
- Discomfort or pain, especially when straining
- Feeling of weakness in the affected area
5. Femoral Hernia
A femoral hernia is less common and occurs when tissue pushes through the femoral canal, near the upper thigh and groin. These hernias are more common in women and can lead to serious complications if left untreated.
Symptoms:
- Swelling or lump near the upper thigh
- Groin discomfort or pressure
- Pain when standing, lifting, or straining
When Is Hernia Surgery Necessary?
While some small hernias can be managed with watchful waiting, surgery is often recommended when:
- The hernia causes pain or discomfort that affects daily activities.
- The hernia continues to grow in size over time.
- There is a risk of incarceration (when the hernia becomes trapped and cannot be pushed back in).
- There is a risk of strangulation (when the blood supply to the herniated tissue is cut off, leading to tissue death and requiring emergency surgery).
Surgical Treatment Options for Hernia Repair
Hernia repair surgery can be performed using different approaches, depending on the size, location, and severity of the hernia.
1. Open Hernia Repair
In an open hernia repair, the surgeon makes an incision near the hernia and pushes the bulging tissue back into place. The weakened area is then reinforced with sutures or surgical mesh to prevent recurrence.
Advantages:
- Effective for larger or complex hernias
- Can be performed under local anesthesia in some cases
Disadvantages:
- Longer recovery time compared to minimally invasive techniques
- Higher risk of post-operative pain
2. Laparoscopic Hernia Repair (Minimally Invasive)
Laparoscopic hernia repair is a minimally invasive technique where small incisions are made, and a tiny camera (laparoscope) is used to guide the repair.
Advantages:
- Smaller incisions and minimal scarring
- Reduced post-operative pain
- Faster recovery and quicker return to daily activities
Disadvantages:
- Requires general anesthesia
- May not be suitable for large or complicated hernias
3. Robotic-Assisted Hernia Repair
A robotic-assisted hernia repair is similar to laparoscopic surgery but uses robotic technology for enhanced precision and control.
Advantages:
- Increased precision for complex hernia repairs
- Less post-operative pain
- Faster recovery time
Disadvantages:
- More expensive than traditional surgery
- Requires specialized surgical expertise
Recovery After Hernia Surgery
Recovery times vary depending on the type of surgery performed. Here’s what most patients can expect:
- Hospital Stay: Most laparoscopic and robotic hernia surgeries are outpatient procedures, allowing patients to go home the same day.
- Pain Management: Mild to moderate discomfort is expected after surgery, but over-the-counter pain medications are often sufficient.
- Physical Activity: Light activity is encouraged, but patients should avoid heavy lifting and strenuous exercise for 4–6 weeks.
- Diet and Hydration: A balanced diet rich in fiber helps prevent constipation, which can strain the surgical site.
- Follow-Up Care: Regular check-ups ensure proper healing and prevent complications.
Preventing Hernia Recurrence
To reduce the risk of hernia recurrence after surgery:
- Maintain a healthy weight to reduce pressure on the abdominal wall.
- Avoid heavy lifting or use proper lifting techniques.
- Incorporate core-strengthening exercises to improve abdominal muscle strength.
- Eat a high-fiber diet to prevent constipation and reduce straining.
- Follow post-surgical activity guidelines provided by your doctor.
Hernia Repair Surgery Conclusion: Choosing the Best Treatment for You
Hernia repair surgery is a safe and effective solution for treating hernias, preventing complications, and improving overall quality of life. Minimally invasive techniques, such as laparoscopic and robotic-assisted surgery, offer faster recovery and less discomfort, making them preferred options for many patients.
If you or a loved one is experiencing hernia symptoms, it’s essential to consult an experienced surgeon to discuss the best treatment approach. At Lenox Hill Surgeons, our team specializes in advanced hernia repair techniques, ensuring the best possible outcomes for our patients. Contact us today to schedule a consultation and explore your options.
Contact Information
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
The Connection Between Mental Health and Surgical Recovery: How Stress Impacts Healing
 What is the connection between mental health and surgical recovery? The body and mind are deeply connected, and this relationship plays a crucial role in surgical recovery. While most people focus on the physical aspects of healing, such as pain management and wound care, mental health also significantly impacts recovery outcomes. Stress, anxiety, and depression can slow down the body’s ability to heal, increase post-operative complications, and even affect pain perception.
What is the connection between mental health and surgical recovery? The body and mind are deeply connected, and this relationship plays a crucial role in surgical recovery. While most people focus on the physical aspects of healing, such as pain management and wound care, mental health also significantly impacts recovery outcomes. Stress, anxiety, and depression can slow down the body’s ability to heal, increase post-operative complications, and even affect pain perception.
Understanding the link between mental health and surgical recovery can help patients take proactive steps to support their healing journey. This guide explores how stress affects the body post-surgery, the importance of mental well-being in recovery, and practical strategies for improving both mental and physical health during the healing process.
How Stress Affects the Body During Surgical Recovery
When the body experiences stress—whether due to anxiety, fear, or emotional distress—it activates the sympathetic nervous system, triggering the fight-or-flight response. While this reaction is essential for survival, prolonged stress after surgery can have negative effects on recovery.
1. Increased Inflammation and Delayed Wound Healing
Chronic stress leads to increased levels of cortisol, a hormone that can suppress the immune system and slow down wound healing. Elevated stress levels can:
- Reduce the body’s ability to fight infections
- Delay the formation of new tissue
- Increase the risk of surgical complications, such as wound dehiscence (reopening of the incision)
2. Heightened Pain Perception
Stress and anxiety can amplify pain perception, making post-operative pain feel more intense than it actually is. Research suggests that patients who struggle with high levels of stress often require higher doses of pain medication and may experience longer-lasting discomfort compared to those with a positive mental outlook.
3. Increased Risk of Post-Surgical Complications
Unmanaged stress can increase the risk of post-operative complications, including:
- High blood pressure and increased heart rate
- Gastrointestinal distress (such as nausea and constipation)
- Reduced appetite, leading to poor nutrition and slower tissue repair
- Higher likelihood of developing chronic pain syndromes
4. Weakened Immune Function
The immune system plays a critical role in preventing post-surgical infections. Chronic stress weakens immune function, leaving the body more susceptible to wound infections, pneumonia, and other post-operative complications.
The Role of Mental Health in a Smooth Recovery
A positive mental outlook and effective stress management can significantly improve surgical outcomes. Patients who actively care for their mental health tend to heal faster, experience less pain, and return to daily activities more quickly.
1. The Power of Positive Thinking
Studies show that optimism and emotional resilience contribute to better surgical outcomes. Patients who believe in their ability to recover tend to:
- Experience faster healing
- Have lower levels of post-operative pain
- Require fewer pain medications
- Have fewer complications
2. Anxiety and Depression Management
Patients who struggle with preoperative anxiety or depression may face greater difficulties during recovery. If left unaddressed, these conditions can:
- Interfere with adherence to post-surgical care instructions
- Lead to sleep disturbances, which slow healing
- Contribute to increased pain perception and longer recovery times
Seeking mental health support before and after surgery can make a significant difference in the recovery process.
Practical Strategies to Reduce Stress and Improve Recovery
Taking proactive steps to manage stress and mental health can improve surgical outcomes. Below are effective strategies to promote healing:
1. Mindfulness and Relaxation Techniques
Practicing mindfulness and relaxation exercises can help reduce stress and promote a sense of calm during the recovery process. Techniques include:
- Deep Breathing Exercises: Helps reduce anxiety and stabilize heart rate.
- Meditation and Guided Imagery: Encourages a positive mindset and reduces pain perception.
- Progressive Muscle Relaxation: Reduces tension and promotes relaxation.
2. Support from Loved Ones
Having a strong support system during recovery is essential for both emotional and physical well-being. Studies show that patients with active social support:
- Recover faster
- Have fewer post-surgical complications
- Experience lower levels of stress and pain
Tip: Lean on family, friends, or a support group to stay motivated and emotionally balanced during recovery.
3. Adequate Sleep and Rest
Sleep is essential for tissue repair, immune function, and overall healing. To improve sleep quality:
- Stick to a regular sleep schedule
- Avoid caffeine and screens before bedtime
- Practice relaxation techniques before bed
- Keep your sleeping environment quiet and comfortable
4. Healthy Nutrition
Eating a well-balanced diet can help the body recover more efficiently. Essential nutrients for healing include:
- Protein: Aids in tissue repair and muscle recovery
- Vitamin C: Supports wound healing and boosts the immune system
- Zinc: Helps with tissue growth and repair
- Omega-3 Fatty Acids: Reduce inflammation and promote healing
5. Light Physical Activity
Engaging in light movement and stretching (as recommended by your surgeon) can:
- Improve circulation and promote healing
- Reduce stiffness and muscle weakness
- Lower stress levels
Tip: Simple activities like short walks and gentle stretching can make a significant difference in recovery speed.
Seeking Professional Support for a Smooth Recovery
If you’re struggling with anxiety, depression, or stress-related symptoms before or after surgery, seeking help from a mental health professional can be beneficial. Some options include:
- Talking to a therapist or counselor for emotional support
- Practicing Cognitive Behavioral Therapy (CBT) to change negative thought patterns
- Joining a post-surgery support group
Mental Health and Surgical Recovery: Prioritizing Mental Health for Better Surgical Outcomes
The connection between mental health and surgical recovery is undeniable. Stress, anxiety, and depression can slow down healing, increase pain perception, and lead to post-surgical complications. By adopting stress-reducing techniques, maintaining a positive mindset, and seeking social and professional support, patients can enhance their healing process and improve overall well-being.
If you or a loved one is preparing for surgery, don’t underestimate the power of mental health in the recovery process. A holistic approach that prioritizes both physical and emotional well-being leads to better outcomes and faster healing.
For expert guidance on pre-surgical preparation and post-operative recovery, the experienced team at Lenox Hill Surgeons is here to support you. Schedule a consultation today to learn how our comprehensive care approach can help you achieve optimal surgical recovery.
Contact Information
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Celiac Disease and Gastrointestinal Surgery: When Is Surgical Intervention Needed?
 Celiac disease is a chronic autoimmune disorder in which the ingestion of gluten triggers an immune response that damages the small intestine. Over time, this damage can lead to malabsorption of nutrients, digestive discomfort, and other serious health complications. While most people with celiac disease manage their condition with a strict gluten-free diet, some individuals experience severe complications that may require surgical intervention.
Celiac disease is a chronic autoimmune disorder in which the ingestion of gluten triggers an immune response that damages the small intestine. Over time, this damage can lead to malabsorption of nutrients, digestive discomfort, and other serious health complications. While most people with celiac disease manage their condition with a strict gluten-free diet, some individuals experience severe complications that may require surgical intervention.
In this guide, we will explore the symptoms and complications of celiac disease, when surgery may be necessary, and the types of procedures that can help manage severe cases.
Understanding Celiac Disease
Celiac disease is caused by an immune reaction to gluten, a protein found in wheat, barley, and rye. When individuals with celiac disease consume gluten, their immune system attacks the lining of the small intestine, damaging the villi—small finger-like projections that absorb nutrients. Over time, this damage leads to malnutrition and various digestive and systemic health issues.
Common Symptoms of Celiac Disease
- Chronic diarrhea or constipation
- Abdominal pain and bloating
- Unexplained weight loss
- Fatigue and weakness
- Iron-deficiency anemia
- Osteoporosis or bone pain
- Skin rash (dermatitis herpetiformis)
- Neurological symptoms (brain fog, headaches, depression)
A gluten-free diet is the only known treatment for celiac disease. However, in some cases, ongoing damage to the intestines or severe complications may require surgical intervention.
When Is Surgery Needed for Celiac Disease?
Surgery is not a standard treatment for celiac disease itself but may be required when complications arise. Below are some of the most common reasons individuals with celiac disease may require surgical intervention.
1. Intestinal Damage Leading to Strictures
Long-term inflammation from untreated celiac disease can cause scarring and narrowing of the small intestine, a condition known as a stricture. Strictures can obstruct food passage, leading to severe digestive issues, including pain, nausea, and vomiting.
When Surgery Is Needed:
- Strictureplasty: This procedure widens the narrowed section of the intestine without removing any portion.
- Bowel Resection: If the strictured section is too damaged, the affected portion of the intestine may be removed.
2. Small Intestinal Cancer
Individuals with long-term, untreated celiac disease have an increased risk of developing small bowel adenocarcinoma, a rare but serious cancer of the small intestine. Symptoms may include unexplained weight loss, persistent abdominal pain, and blood in the stool.
When Surgery Is Needed:
- Segmental Resection: Removal of the affected section of the small intestine.
- Colectomy: If cancer has spread to the colon, partial or total colectomy may be necessary.
3. Refractory Celiac Disease
Refractory celiac disease (RCD) occurs when symptoms persist despite strict adherence to a gluten-free diet. In some cases, RCD progresses to enteropathy-associated T-cell lymphoma (EATL), a rare but aggressive cancer.
When Surgery Is Needed:
- Intestinal Biopsy and Resection: If lymphoma or other malignancies develop, surgical removal of the affected tissue may be required.
- Intestinal Transplant (Rare): In extreme cases where severe intestinal damage prevents normal digestion, an intestinal transplant may be considered.
4. Severe Ulcers and Perforation
Chronic inflammation from celiac disease can cause intestinal ulcers that may lead to perforation (a hole in the intestinal wall). This is a medical emergency that requires immediate surgical intervention.
When Surgery Is Needed:
- Emergency Bowel Repair: The perforated section of the intestine is repaired to prevent infection.
- Partial Small Bowel Resection: If the perforation is extensive, part of the intestine may need to be removed.
Surgical Options for Celiac-Related Complications
When surgery is necessary, various techniques are used depending on the complication. Some of the most common surgical procedures include:
- Strictureplasty: A procedure that widens a narrowed segment of the small intestine without removing any portion.
- Bowel Resection: Removal of a diseased section of the intestine, often followed by reconnection of the remaining portions.
- Colectomy: Removal of part or all of the colon if complications extend beyond the small intestine.
- Emergency Surgery for Perforation: Immediate repair of a perforated intestine to prevent life-threatening infections.
- Intestinal Transplant: A rare procedure for individuals with irreversible intestinal failure.
Minimally Invasive Surgery for Celiac Disease Complications
Whenever possible, surgeons opt for minimally invasive techniques, which provide several advantages:
- Smaller incisions and less scarring
- Reduced post-operative pain
- Shorter hospital stays and faster recovery
- Lower risk of infection and complications
Techniques such as laparoscopic surgery and robotic-assisted surgery are commonly used for bowel resections and strictureplasty.
Recovery After GI Surgery for Celiac Disease
Recovery after surgery depends on the specific procedure and the patient’s overall health. In general, most patients can expect:
- Hospital Stay: Depending on the surgery, hospitalization may last from a few days to a few weeks.
- Dietary Adjustments: A gradual return to solid foods is recommended, often beginning with a liquid or soft diet.
- Pain Management: Pain medications may be prescribed to manage discomfort.
- Activity Restrictions: Patients should avoid strenuous activities for several weeks while healing.
- Follow-Up Care: Regular check-ups with a gastroenterologist and surgeon ensure proper healing and monitor for complications.
When to Seek Medical Attention
Individuals with celiac disease should consult a doctor if they experience:
- Persistent or worsening abdominal pain
- Unintentional weight loss
- Severe bloating and vomiting
- Blood in the stool or black, tarry stools
- Difficulty swallowing or severe acid reflux
Early intervention can help prevent complications and improve long-term outcomes.
Conclusion: Managing Celiac Disease and When Surgery Is Necessary
While most individuals with celiac disease can manage their condition through a strict gluten-free diet, complications can arise that may require surgical intervention. Strictures, cancer, refractory celiac disease, and intestinal perforations are serious conditions that should not be ignored.
If you or a loved one are experiencing severe gastrointestinal symptoms related to celiac disease, consult with a gastroenterologist or a specialized surgeon to explore your treatment options. Early detection and appropriate surgical intervention can improve quality of life and prevent life-threatening complications.
For expert evaluation and advanced surgical care in Manhattan, contact Lenox Hill Surgeons today to schedule a consultation.
Contact Information
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
When Do You Need Surgery for Irritable Bowel Syndrome (IBS) & Other GI Conditions
When do you need to consider surgery for Irritable Bowel Syndrome & other serious GI conditions? Irritable Bowel Syndrome (IBS) is a common digestive disorder that affects millions of people worldwide. While IBS can cause significant discomfort, it is generally a functional disorder, meaning it does not cause structural damage to the digestive tract. However, certain gastrointestinal (GI) conditions present with similar symptoms but may be far more serious, requiring medical intervention, including surgery.
Distinguishing between IBS and more severe GI disorders is essential for receiving the appropriate treatment. This guide explores the differences between IBS and conditions that may require surgery, how to recognize red-flag symptoms, and when surgical intervention becomes necessary.

Understanding IBS: Symptoms and Management
IBS is a chronic disorder that affects how the intestines function. It is often triggered by stress, diet, hormonal changes, or infections. While it does not cause lasting damage to the intestines, it can significantly impact a person’s quality of life.
Common Symptoms of IBS
- Abdominal pain or cramping, often relieved by bowel movements
- Bloating and excessive gas
- Diarrhea, constipation, or alternating between both
- Mucus in the stool
- Feeling of incomplete bowel movements
- Symptoms that fluctuate over time and are triggered by certain foods or stress
How IBS Is Managed
Because IBS is a functional disorder, treatment focuses on symptom management through lifestyle and dietary changes, including:
- Dietary Modifications: Avoiding trigger foods such as high-fat foods, caffeine, dairy, and artificial sweeteners can reduce symptoms.
- Fiber Intake: Increasing fiber can help regulate bowel movements, but some individuals may need to limit insoluble fiber.
- Stress Management: Practicing relaxation techniques such as yoga, meditation, and deep breathing can help reduce symptom flare-ups.
- Medications: Anti-diarrheal medications, laxatives, antispasmodics, or probiotics may be prescribed depending on the individual’s symptoms.
Serious GI Conditions That May Require Surgery
While IBS does not cause structural damage, other gastrointestinal conditions can have similar symptoms but require more advanced treatment, including surgery.
1. Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) includes Crohn’s disease and ulcerative colitis, both of which involve chronic inflammation of the digestive tract. Unlike IBS, IBD can cause permanent damage to the intestines.
Symptoms That Differentiate IBD from IBS:
- Persistent diarrhea, sometimes with blood or mucus
- Severe abdominal pain and cramping
- Unintentional weight loss
- Fever and extreme fatigue
- Delayed growth in children
When Surgery Is Needed for IBD:
- Bowel Resection: In cases of Crohn’s disease, diseased portions of the intestine may need to be removed.
- Colectomy: For ulcerative colitis, removing part or all of the colon may be necessary.
- Ileostomy or Colostomy: A surgical opening (stoma) may be created if the intestines cannot be reconnected.
2. Colorectal Cancer
Colorectal cancer can develop from polyps in the colon or rectum, and early symptoms may mimic IBS. However, unlike IBS, colorectal cancer can be life-threatening if left untreated.
Symptoms That Differentiate Colorectal Cancer from IBS:
- Rectal bleeding or blood in the stool
- Persistent changes in bowel habits
- Unexplained weight loss
- Fatigue and weakness
- Persistent abdominal pain
When Surgery Is Needed for Colorectal Cancer:
- Polypectomy: Small cancerous polyps can be removed during a colonoscopy.
- Colectomy: Part or all of the colon may be removed if cancer has spread.
- Colostomy or Ileostomy: In some cases, a stoma is required for waste elimination.
3. Diverticulitis
Diverticulitis occurs when small pouches (diverticula) in the colon become inflamed or infected, causing severe abdominal pain.
Symptoms That Differentiate Diverticulitis from IBS:
- Severe lower abdominal pain, often on the left side
- Fever and chills
- Nausea and vomiting
- Changes in bowel movements, often with constipation
When Surgery Is Needed for Diverticulitis:
- Bowel Resection: If diverticulitis recurs frequently or causes complications like perforations or abscesses, the affected section of the colon may be removed.
- Colostomy: If inflammation is severe, a temporary or permanent colostomy may be necessary.
4. Intestinal Obstructions
Intestinal obstructions can occur due to scar tissue, hernias, tumors, or severe inflammation. Unlike IBS, obstructions can be life-threatening and require immediate medical attention.
Symptoms That Indicate an Obstruction:
- Severe abdominal pain and bloating
- Inability to pass gas or have a bowel movement
- Persistent nausea and vomiting
- Swelling of the abdomen
When Surgery Is Needed for an Obstruction:
- Bowel Resection: The blocked or damaged portion of the intestine is removed.
- Strictureplasty: A procedure used to widen a narrowed section of the intestine.
When to See a Doctor
 If you have persistent GI symptoms, it’s essential to consult a healthcare provider. While IBS is not life-threatening, other conditions that mimic IBS can be serious. Seek medical attention if you experience:
If you have persistent GI symptoms, it’s essential to consult a healthcare provider. While IBS is not life-threatening, other conditions that mimic IBS can be serious. Seek medical attention if you experience:
- Unexplained weight loss
- Severe abdominal pain that does not improve
- Blood in the stool or rectal bleeding
- Persistent vomiting or inability to eat
- Symptoms that worsen over time or do not respond to treatment
Surgery for Irritable Bowel Syndrome & Other Serious GI Conditions: Conclusion
While IBS is a manageable condition that does not require surgery, many serious GI conditions share similar symptoms. Recognizing the warning signs of IBD, colorectal cancer, diverticulitis, or intestinal obstructions is essential for timely diagnosis and treatment.
If you are experiencing persistent digestive symptoms and are unsure of the cause, consulting a specialist can help determine whether surgery is necessary. For expert evaluation and advanced surgical care in Manhattan, contact Lenox Hill Surgeons today.
Contact Information
LENOX HILL SURGEONS
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Cancer Prevention and Early Detection: How Surgery Can Play a Life-Saving Role
What role does surgery play in cancer prevention and early detection? Cancer remains one of the leading causes of death worldwide, but advancements in medical science have significantly improved the ability to detect and treat it early. One of the most effective ways to combat cancer is through prevention and early detection, which can dramatically increase survival rates.
Surgery plays a crucial role in both preventing certain types of cancer and treating early-stage cancers before they spread. This guide will explore how surgery is used for cancer prevention, the importance of early detection, and how surgical interventions can be life-saving.

The Importance of Cancer Prevention
While some cancers develop due to genetic predisposition, many are preventable through lifestyle changes and proactive medical interventions. Taking steps to reduce risk factors and undergo regular screenings can significantly lower the likelihood of developing cancer.
Key Cancer Prevention Strategies
- Avoid Tobacco: Smoking is the leading cause of lung cancer and contributes to cancers of the throat, mouth, pancreas, and bladder. Avoiding tobacco significantly reduces cancer risk.
- Maintain a Healthy Diet: Eating a diet rich in fruits, vegetables, whole grains, and lean proteins while limiting processed foods and red meats can help lower cancer risk.
- Exercise Regularly: Engaging in physical activity helps maintain a healthy weight, reducing the risk of cancers like breast, colon, and endometrial cancer.
- Limit Alcohol Consumption: Excessive alcohol use increases the risk of cancers in the liver, breast, throat, and colon. Moderation is key.
- Protect Yourself from the Sun: Skin cancer, including melanoma, is often caused by excessive UV exposure. Wearing sunscreen and protective clothing can reduce the risk.
- Get Vaccinated: Certain cancers, such as cervical and liver cancer, are linked to viruses like HPV and hepatitis B. Vaccination can help prevent these infections.
- Undergo Regular Screenings: Detecting cancer in its early stages can save lives. Screenings like mammograms, Pap smears, colonoscopies, and prostate exams are critical.
How Surgery Plays a Role in Cancer Prevention
For individuals at high risk of developing cancer, surgery can be used as a preventive measure to remove tissue that has a high likelihood of becoming cancerous. This is known as prophylactic surgery or risk-reducing surgery.
Common Preventive Surgeries for Cancer
- Prophylactic Mastectomy: Women with a strong family history of breast cancer or BRCA gene mutations may choose to have their breasts removed to reduce their risk of developing cancer.
- Prophylactic Oophorectomy: The removal of the ovaries can help prevent ovarian cancer in women at high genetic risk.
- Colon Polyp Removal: In individuals with a history of polyps or familial adenomatous polyposis (FAP), removing polyps during a colonoscopy or performing a colectomy can prevent colorectal cancer.
- Thyroidectomy: For individuals with genetic predisposition to thyroid cancer, removing the thyroid before cancer develops can be a proactive strategy.
- Hysterectomy: Women with a high risk of uterine or cervical cancer may undergo a hysterectomy (removal of the uterus) to eliminate the risk.
The Role of Surgery in Early Cancer Detection
Early cancer detection allows for more effective treatment and a higher chance of survival. In some cases, surgical procedures are used to detect cancerous or pre-cancerous tissues.
Diagnostic Surgical Procedures
- Biopsy: A biopsy is a procedure where a small sample of tissue is removed and analyzed to check for cancerous cells. This is commonly used for breast lumps, suspicious skin lesions, and enlarged lymph nodes.
- Endoscopic Surgery: Using a flexible tube with a camera, surgeons can remove small tissue samples from the digestive tract, lungs, or bladder for examination.
- Lymph Node Dissection: In cases where cancer is suspected to have spread, nearby lymph nodes may be surgically removed and examined to determine the extent of the disease.

Surgical Treatment for Early-Stage Cancers
If cancer is detected at an early stage, surgery is often the primary treatment. Removing tumors before they have a chance to spread can significantly improve survival rates.
Common Surgeries for Early-Stage Cancer
- Lumpectomy: A lumpectomy removes a tumor while preserving the rest of the breast. This is an effective treatment for early-stage breast cancer.
- Colectomy: For colon cancer detected in its early stages, removing part or all of the colon may prevent the spread of cancerous cells.
- Prostatectomy: A prostatectomy removes the prostate gland in men diagnosed with localized prostate cancer.
- Partial or Total Nephrectomy: In early-stage kidney cancer, a nephrectomy removes part or all of the affected kidney to prevent further tumor growth.
- Skin Cancer Excision: Early-stage melanoma and other skin cancers can be surgically removed before they spread deeper into the skin layers.
Minimally Invasive Surgery for Cancer Treatment
Advancements in surgical technology now allow for minimally invasive procedures, reducing recovery time and improving patient outcomes. Many cancer surgeries can now be performed using laparoscopy or robotic-assisted surgery, which offer numerous benefits:
- Smaller incisions and reduced scarring
- Shorter hospital stays and faster recovery times
- Lower risk of infection and complications
- More precise removal of cancerous tissue with robotic-assisted surgery
Recovery and Post-Surgical Care
Following cancer surgery, patients may need additional treatments such as radiation therapy, chemotherapy, or immunotherapy to ensure all cancer cells are eliminated. Recovery varies depending on the type of procedure, but most patients can expect:
- Hospital stays ranging from a few days to a week, depending on the procedure
- Pain management with medication
- Follow-up appointments to monitor for any signs of recurrence
- Rehabilitation and physical therapy for certain types of cancer surgeries
- Emotional and psychological support, as cancer treatment can be both physically and mentally challenging
Cancer Prevention and Early Detection: Conclusion
Cancer prevention and early detection are essential in reducing cancer-related deaths. By making healthy lifestyle choices, undergoing regular screenings, and seeking medical advice when symptoms arise, individuals can take proactive steps in reducing their cancer risk. For those at high risk, preventive surgeries can provide peace of mind and significantly lower the chances of developing certain cancers.
If you or a loved one have concerns about cancer risk, early detection, or surgical treatment options, consulting with a qualified general surgeon can provide clarity and guidance. Early intervention saves lives.
For expert consultation and state-of-the-art surgical care in Manhattan, contact Lenox Hill Surgeons today to schedule an appointment.
Contact Information
LENOX HILL SURGEONS LLP
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
lenoxhillsurgeons@gmail.com
Visit our website for more information:
https://lenoxhillsurgeons.com/
Traumatic Brain Injury and Surgery: When Is Surgical Intervention Necessary?
Traumatic brain injury (TBI) is a serious medical condition that occurs when an external force injures the brain. It can result from falls, vehicle accidents, sports injuries, or violent incidents. While mild TBIs, such as concussions, often heal with rest and medical observation, severe cases may require surgical intervention to prevent further brain damage, relieve pressure, and improve the chances of recovery.
March is Traumatic Brain Injury Awareness Month, making it an essential time to discuss how surgical treatment plays a crucial role in managing severe brain injuries. This guide explores when surgery is necessary, the different types of surgical procedures, and what patients and families can expect during recovery.

Understanding Traumatic Brain Injury
TBI is classified based on severity, which can range from mild to severe. Mild TBIs, often referred to as concussions, typically cause temporary symptoms such as headaches, dizziness, and confusion. Moderate to severe TBIs, however, can lead to long-term complications, cognitive impairment, and in some cases, life-threatening conditions.
Common causes of TBI include direct trauma to the head, rapid acceleration or deceleration (such as in car accidents), and penetrating injuries from objects like bullets or shrapnel. Symptoms can vary but may include loss of consciousness, seizures, slurred speech, memory loss, and profound confusion.
When Is Surgery Necessary for TBI?
Not all TBIs require surgical intervention, but in certain cases, surgery becomes a life-saving procedure. The primary reasons a patient may need brain surgery after a traumatic injury include:
- Hematomas and Brain Bleeds: A collection of blood, known as a hematoma, can form in or around the brain due to trauma. If the hematoma is large or rapidly expanding, it can increase intracranial pressure and may need to be surgically removed.
- Skull Fractures: Some skull fractures, especially depressed skull fractures where bone fragments press into the brain, require surgery to repair the skull and prevent further damage.
- Brain Swelling (Edema): Following a severe injury, the brain may swell, increasing pressure inside the skull. Surgery may be required to relieve this pressure and prevent brain damage.
- Penetrating Brain Injuries: Objects that penetrate the skull, such as bullets or sharp debris, may require surgical removal to prevent infection and further trauma.
- Hydrocephalus: This condition, where cerebrospinal fluid builds up in the brain, can occur after a TBI. A surgical procedure may be needed to drain excess fluid and relieve pressure.
Types of Surgical Procedures for TBI
Depending on the severity and nature of the brain injury, different surgical techniques may be used to stabilize the patient and improve outcomes. Below are the most common types of brain surgeries performed for TBI:
1. Craniotomy
A craniotomy is a surgical procedure where a section of the skull is temporarily removed to access the brain. This procedure is performed to remove blood clots, stop bleeding, or relieve swelling. After the surgery, the bone flap is typically replaced.
2. Decompressive Craniectomy
In cases of severe brain swelling, a decompressive craniectomy may be performed. This procedure involves removing part of the skull to give the swollen brain room to expand, reducing pressure and preventing further damage. The removed skull section is often stored and reattached once swelling subsides.
3. Hematoma Removal
If a large hematoma forms inside or outside the brain, surgery may be required to remove the clot. This helps relieve pressure and prevents additional damage to brain tissue.
4. Skull Fracture Repair
Surgery may be needed to correct depressed skull fractures, where broken bone fragments press into the brain. The surgeon will reposition the bone fragments or replace them with artificial materials if necessary.
5. Ventriculostomy and Shunt Placement
For cases of hydrocephalus, where cerebrospinal fluid builds up in the brain, a ventriculostomy may be performed. This procedure involves placing a catheter in the brain’s ventricles to drain excess fluid. Alternatively, a shunt may be implanted to divert fluid to another part of the body for absorption.

Recovery and Rehabilitation After Brain Surgery
Recovering from brain surgery after a TBI varies depending on the severity of the injury and the type of procedure performed. The immediate goals of treatment focus on stabilizing the patient, preventing further complications, and beginning rehabilitation.
Hospitalization and Immediate Post-Surgery Care
After surgery, patients are closely monitored in an intensive care unit (ICU) to manage swelling, prevent infection, and ensure stable brain function. Some patients may require ventilators to assist with breathing, and imaging tests (CT scans or MRIs) are performed to assess healing.
Rehabilitation Process
Rehabilitation is a crucial part of recovery, especially for patients with cognitive or motor impairments following surgery. Common rehabilitation therapies include:
- Physical Therapy: Helps patients regain movement, strength, and coordination.
- Occupational Therapy: Focuses on relearning daily activities such as dressing, eating, and writing.
- Speech Therapy: Aids in improving communication and swallowing functions for patients affected by brain trauma.
- Cognitive Therapy: Supports memory, problem-solving, and emotional regulation after a brain injury.
Long-Term Outlook for TBI Patients
The long-term prognosis for TBI patients depends on factors such as the severity of the injury, the speed of medical intervention, and the effectiveness of rehabilitation. Some individuals make a full recovery, while others may experience lasting cognitive or physical impairments.
Regular follow-ups with neurosurgeons and neurologists help monitor progress and address any complications that may arise, such as seizures, personality changes, or ongoing headaches. Many patients benefit from ongoing therapy and support from family members and caregivers.
Preventing Traumatic Brain Injuries
While not all TBIs can be prevented, certain precautions can reduce the risk of serious head injuries:
- Always wear a seatbelt while driving and ensure children are in properly secured car seats.
- Use helmets when participating in contact sports, cycling, or riding motorcycles.
- Ensure living spaces are free of tripping hazards to prevent falls, especially for older adults.
- Avoid risky behaviors, such as driving under the influence of alcohol or engaging in high-risk activities without proper safety measures.
- Educate children and athletes about the dangers of head injuries and the importance of reporting symptoms after a blow to the head.
Conclusion: Seeking Immediate Care for TBI
Traumatic brain injuries can have life-altering consequences, and timely medical attention is critical in preventing further damage. While not all TBIs require surgery, those that do often involve complex procedures aimed at saving lives and preserving brain function.
If you or a loved one experiences a traumatic head injury, seek immediate medical attention. Early intervention and expert surgical care can significantly improve the chances of recovery.
For those in need of specialized surgical treatment for traumatic brain injuries in Manhattan, contact Lenox Hill Surgeons today to schedule a consultation and learn more about our advanced neurosurgical care.
Contact Information
LENOX HILL SURGEONS LLP
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
Dr.Ginberg@lenoxhillsurgeons.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Colorectal Cancer Awareness: The Importance of Screening and Surgical Treatment Options
 Since March is Colorectal Cancer Awareness Month, it’s the perfect time to educate individuals about the importance of regular screenings and the role surgery plays in treating this disease. Colorectal cancer is one of the most common cancers worldwide, affecting both men and women. Early detection through routine screening and timely surgical intervention can significantly improve survival rates and prevent complications.
Since March is Colorectal Cancer Awareness Month, it’s the perfect time to educate individuals about the importance of regular screenings and the role surgery plays in treating this disease. Colorectal cancer is one of the most common cancers worldwide, affecting both men and women. Early detection through routine screening and timely surgical intervention can significantly improve survival rates and prevent complications.
This guide will cover colorectal cancer risk factors, screening methods, and surgical treatment options to help patients understand their choices for prevention and treatment.
Understanding Colorectal Cancer: Risk Factors and Symptoms
Colorectal cancer begins in the colon or rectum and often develops from abnormal growths known as polyps. While some polyps remain benign, others can turn cancerous over time, making early detection crucial.
Risk Factors for Colorectal Cancer
Certain factors can increase the risk of developing colorectal cancer. These include:
- Age: The majority of colorectal cancer cases occur in individuals over the age of 50.
- Family History: A family history of colorectal cancer or polyps increases the risk of developing the disease.
- Diet: A diet high in red and processed meats and low in fiber has been linked to an increased risk.
- Obesity and Sedentary Lifestyle: Lack of physical activity and excess body weight can contribute to higher cancer risk.
- Smoking and Alcohol Use: Heavy alcohol consumption and smoking are associated with a greater risk of colorectal cancer.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis increase the likelihood of colorectal cancer.
Common Symptoms of Colorectal Cancer
Colorectal cancer symptoms often appear in the later stages, making regular screening vital for early detection. Some common symptoms include:
- Persistent changes in bowel habits, including diarrhea or constipation
- Blood in the stool or rectal bleeding
- Unexplained weight loss
- Abdominal discomfort, cramps, or bloating
- Fatigue and weakness
- A feeling of incomplete bowel movements
Since these symptoms can be caused by various conditions, it’s essential to consult a healthcare provider for proper evaluation.

The Importance of Colorectal Cancer Screening
Screening tests help detect colorectal cancer early, often before symptoms appear. When detected in its early stages, colorectal cancer is highly treatable.
Recommended Screening Methods
The American Cancer Society recommends that individuals at average risk begin colorectal cancer screening at age 45. Those with higher risk factors may need to start screening earlier. Screening options include:
- Colonoscopy: A procedure where a thin, flexible tube with a camera examines the colon and rectum for polyps or cancerous growths. If polyps are found, they can be removed during the procedure.
- Fecal Immunochemical Test (FIT): A non-invasive stool test that detects hidden blood, which may indicate cancer or polyps.
- Stool DNA Test: This test detects abnormal DNA in stool samples, which may indicate colorectal cancer.
- CT Colonography (Virtual Colonoscopy): A special CT scan that provides detailed images of the colon and rectum to check for abnormalities.
- Sigmoidoscopy: A procedure similar to a colonoscopy but only examines the lower part of the colon.
Surgical Treatment Options for Colorectal Cancer
For patients diagnosed with colorectal cancer, surgery is often the primary treatment, especially for localized tumors. The type of surgery performed depends on the size, stage, and location of the tumor.
Types of Colorectal Cancer Surgery
- Polypectomy: If cancer is detected in a polyp during a colonoscopy, it may be removed immediately using specialized instruments.
- Local Excision: Early-stage cancers that haven’t spread beyond the superficial layers of the colon or rectum may be removed using a minimally invasive approach.
- Colectomy: A colectomy involves removing a section of the colon containing the tumor. The healthy ends of the colon are then reconnected.
- Proctectomy: In cases of rectal cancer, part or all of the rectum may be removed, depending on the tumor’s location.
- Colostomy or Ileostomy: If reconnecting the intestines isn’t possible immediately after surgery, a temporary or permanent stoma may be created to allow waste to exit the body.
Minimally Invasive Techniques in Colorectal Surgery
Many colorectal cancer surgeries can now be performed using minimally invasive techniques, reducing recovery time and surgical risks. These approaches include:
- Laparoscopic Surgery: Small incisions are made, and a camera guides the surgeon in removing cancerous tissue with precision.
- Robotic-Assisted Surgery: Robotic technology enhances precision and control, making it an effective option for colorectal procedures.
- Transanal Endoscopic Microsurgery (TEM): A minimally invasive technique used for removing small tumors in the rectum.
Recovery and Post-Surgical Care
Recovery from colorectal surgery depends on the type of procedure performed, the patient’s overall health, and whether complications arise. Patients can expect:
- Hospital Stay: A hospital stay of a few days to a week is typical, depending on the type of surgery.
- Dietary Adjustments: Patients may need to follow a special diet temporarily to allow the digestive system to heal.
- Pain Management: Pain medications are prescribed to manage discomfort after surgery.
- Physical Activity: Light movement is encouraged to prevent blood clots, but strenuous activity should be avoided for several weeks.
- Follow-Up Care: Regular follow-ups with a surgeon and oncologist help monitor recovery and detect any potential recurrence.

Preventing Colorectal Cancer
While surgery is an effective treatment for colorectal cancer, prevention is always the best approach. Some steps to lower your risk include:
- Eating a Healthy Diet: A diet rich in fiber, fruits, and vegetables while limiting red and processed meats can reduce cancer risk.
- Staying Active: Regular physical activity can help lower the risk of colorectal cancer.
- Maintaining a Healthy Weight: Obesity is a known risk factor for colorectal cancer.
- Quitting Smoking and Limiting Alcohol: Reducing tobacco and alcohol use can significantly decrease cancer risk.
- Getting Regular Screenings: Screening is the most effective way to detect colorectal cancer early when it is most treatable.
Conclusion: Take Action for Colorectal Cancer Awareness
Colorectal cancer is a serious but highly preventable disease with early detection and appropriate treatment. Regular screenings, a healthy lifestyle, and timely surgical intervention can significantly improve outcomes and save lives. If you or a loved one are experiencing symptoms or are due for screening, consult with a colorectal specialist today.
For expert colorectal cancer screening and surgical treatment in Manhattan, contact Lenox Hill Surgeons today to schedule a consultation.
Contact Information
LENOX HILL SURGEONS LLP
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
Dr.Ginberg@lenoxhillsurgeons.com
Visit our website for more information: https://lenoxhillsurgeons.com/
Lenox Hill Surgeons LLP, Expert Surgeons in New York City’s Upper East Side
 Welcome to the official blog of Lenox Hill Surgeons LLP, dedicated and highly skilled NYC general surgeons committed to providing exceptional care to patients in New York City. We understand that surgical procedures can be daunting, and our mission is to offer not only cutting-edge surgical expertise but also a compassionate and personalized approach to every individual who walks through our doors.
Welcome to the official blog of Lenox Hill Surgeons LLP, dedicated and highly skilled NYC general surgeons committed to providing exceptional care to patients in New York City. We understand that surgical procedures can be daunting, and our mission is to offer not only cutting-edge surgical expertise but also a compassionate and personalized approach to every individual who walks through our doors.
At Lenox Hill Surgeons LLP, we believe in the power of minimally invasive techniques, utilizing the latest advancements in laparoscopic and robotic surgery to ensure faster recovery times, reduced pain, and minimal scarring. Our surgeons have extensive experience and a dedication to staying at the forefront of surgical innovation.
Meet Our Expert Surgeons
We’re proud to introduce two of our founding partners, Dr. Sergei Dolgopolov and Dr. Roman Grinberg, whose combined experience and commitment to patient care are the cornerstones of our practice.
Dr. Sergei Dolgopolov
 Dr. Dolgopolov brings a wealth of experience and a truly international perspective to Lenox Hill Surgeons. With a distinguished career spanning decades, he graduated with Honors and Science Awards from Sechenov Moscow Medical School in 1983. His surgical training began in urology at Moscow Medical Academy Hospital Center and continued with extensive experience in clinical research and reconstructive surgery at Burdenko Central Military Hospital in Moscow, where he aided war victims.
Dr. Dolgopolov brings a wealth of experience and a truly international perspective to Lenox Hill Surgeons. With a distinguished career spanning decades, he graduated with Honors and Science Awards from Sechenov Moscow Medical School in 1983. His surgical training began in urology at Moscow Medical Academy Hospital Center and continued with extensive experience in clinical research and reconstructive surgery at Burdenko Central Military Hospital in Moscow, where he aided war victims.
Dr. Dolgopolov further honed his skills in the United States, completing a residency and chief residency at SUNY Downstate Health Science Center with Honors. He served as a surgical attending and clinical assistant professor at SUNY Downstate before joining Surgical Associates of New York, LLP, and later, Lenox Hill Surgeons, LLP.
His expertise lies in minimally invasive, laparoscopic, robotic, general, and oncology surgery. He is also an assistant professor of surgery at Mount Sinai School of Medicine and Lenox Hill Hospital, demonstrating his commitment to both patient care and surgical education.
Dr. Roman Grinberg
 Dr. Grinberg is a highly skilled general, minimally invasive, and robotic surgeon affiliated with Lenox Hill Hospital. He earned his medical degree from Russian State Medical University in 1999 and subsequently pursued research at Beth Israel Medical Center in New York City. He completed his general surgery residency at Conemaugh Memorial Medical Center, an affiliate of Temple University School of Medicine, and a minimally invasive fellowship at Staten Island University Hospital.
Dr. Grinberg is a highly skilled general, minimally invasive, and robotic surgeon affiliated with Lenox Hill Hospital. He earned his medical degree from Russian State Medical University in 1999 and subsequently pursued research at Beth Israel Medical Center in New York City. He completed his general surgery residency at Conemaugh Memorial Medical Center, an affiliate of Temple University School of Medicine, and a minimally invasive fellowship at Staten Island University Hospital.
Dr. Grinberg has held faculty positions and served as an Assistant Professor of Surgery at Hofstra University School of Medicine. His passion for minimally invasive and robotic surgery is evident in his dedication to providing the best possible care for his patients.
As Dr. Grinberg states, “My specialty and interest are minimally invasive and robotic general surgery. I sincerely believe that the ability granted to me by the American College of Surgeons, to take care of my patients, is a true gift and a privilege. The knowledge and skills that I have learned during my training, along with my experience and personal qualities as a physician that is truly dedicated to my profession, continues to help me provide the best and most personalized care for each and every patient.”
Our Commitment to You
At Lenox Hill Surgeons, we are dedicated to:
- Providing expert surgical care: Our surgeons are highly trained and experienced in the latest surgical techniques.
- Utilizing minimally invasive procedures: We prioritize minimally invasive approaches whenever possible to reduce recovery time and improve patient outcomes.
- Offering personalized care: We understand that every patient is unique, and we tailor our treatment plans to meet individual needs.1
- Maintaining a compassionate and supportive environment: We strive to create a comfortable and reassuring experience for our patients.
We invite you to explore our website, LenoxHillSurgeons.com, to learn more about our services and our team. We look forward to providing you with the highest quality surgical care.
Stay tuned for future blog posts where we will delve deeper into specific surgical procedures, patient care tips, and advancements in surgical technology.
For More Information or to schedule a consultation, please contact us:
LENOX HILL SURGEONS, LLP
155 East 76th Street
Suite 1C
New York, NY 10021
646-933-3224
Dr.Grinberg@lenoxhillsurgeons.com